INTRODUCTION
Despite advances in image-based evaluation of parenchymal liver disease, a liver biopsy is still needed to determine the etiology or to grade the severity of the disease. The indication for liver biopsy becomes more compelling when a myriad of tests, including serology, imaging, and endoscopy (endoscopic retrograde cholangiopancreatography or endoscopic ultrasound [EUS]), have failed to yield a diagnosis. Traditionally, a percutaneous or transjugular approach is used for sampling of liver tissue [1,2]. More recently, EUS has emerged as an ideal alternative for percutaneous liver biopsy in a subset of patients who would benefit from examination of the upper gastrointestinal tract, pancreas, and the biliary tree, and the surrounding vasculature in addition to visualization of the liver. EUS-guided liver biopsy has gained momentum, as studies have shown that it has comparable diagnostic yield to percutaneous biopsy [3-5]. Newer needle designs have been introduced in parallel to this growing interest. However, few studies have compared the performance of different needle sizes and the needle designs. In this ex vivo study, we compared the performance of 6 latest commercially available needles, including the most recent 19 G (3 needles), 20 G (1 needle), and 22 G (2 needles) models.
MATERIALS AND METHODS
EUS fine-needle biopsy
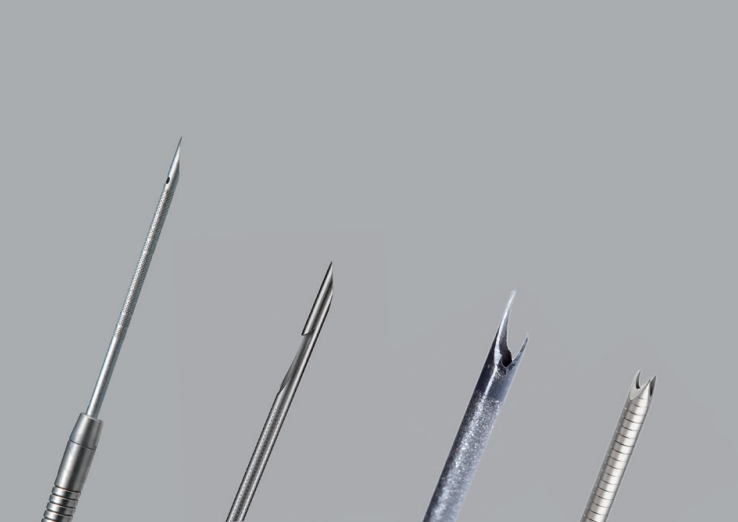
A freshly harvested bovine liver was procured from the University of California Davis Veterinary School Meat Laboratory (offered as a food item) and promptly used for liver biopsies. Six most recent models of commercially available needles were evaluated: Acquire 19 G/22 G (Boston Scientific, Marlborough, MA, USA), SharkCore 19 G/22 G (Medtronic, Minneapolis, MN, USA), EZ Shot 3 Plus 19 G (Olympus America, Center Valley, PA, USA), and EchoTip ProCore 20 G (Cook Medical, Bloomington, IN, USA). These needles vary in size and tip design, as shown in Fig. 1. The Acquire needle is a Franseen-type needle with 3 cutting tips. The SharkCore needle is a fork-tip-type needle with 2 parallel cutting tips. EZ Shot 3 Plus is a Menghini-type needle with a beveled end cutting edge; this needle is made of nitinol and is especially useful in lesions in difficult-to-reach locations, where there is excessive torque on the scope. Lastly, the ProCore needle has an end cutting beveled edge and a core trap near the tip. The advantages of the ProCore needle are flexibility because of its smaller gauge (20 G) and the ability to provide a tissue core specimen owing to the side trap. Each needle was passed through a curvilinear Olympus echoendoscope (GF-UCT140; Olympus America) in a simulated flexed scope position to approximate the real-life tissue acquisition technique (Fig. 2). Real-time imaging was not performed (due to the large target). Five aspirates per needle were obtained with 10 mL of wet suction, resulting in a total of 30 core biopsy specimens. Each aspirate consisted of 5 actuations with 4-cm needle advancement per actuation, performed by a single operator. Separate nonoverlapping locations from both lobes of the liver were chosen for each biopsy.
Specimen preparation and data analysis
The tissue cores were fixed in 10% formalin and processed according to the standard method. Paraffin wax-embedded sections were stained with hematoxylin and eosin (H&E). The H&E slides were scanned at ├Ś20 magnification using an Aperio AT2 scanner (Leica Microsystems GmBH, Wetzlar, Germany). All tissue measurements (total fragments and their lengths) were obtained using the Aperio Image Scope viewer (v12.3.2.8013).
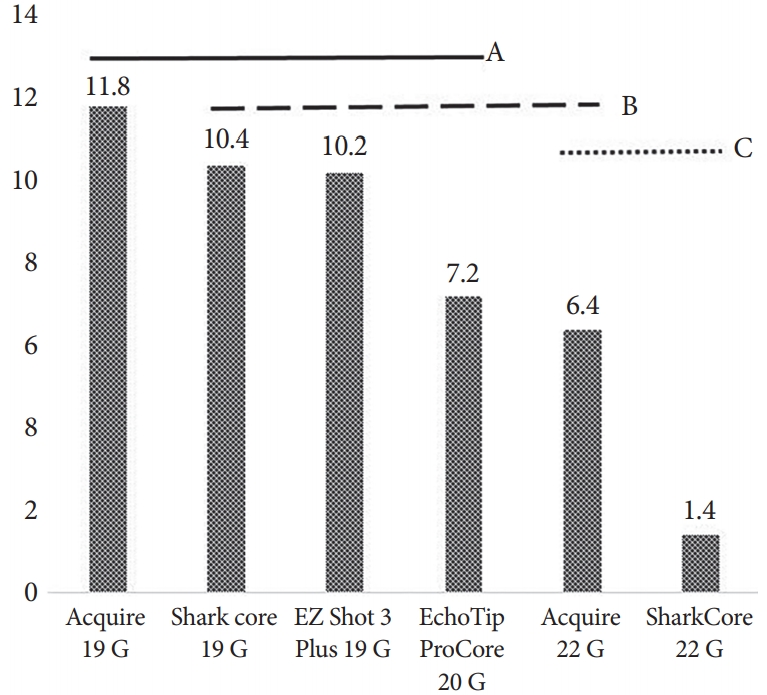
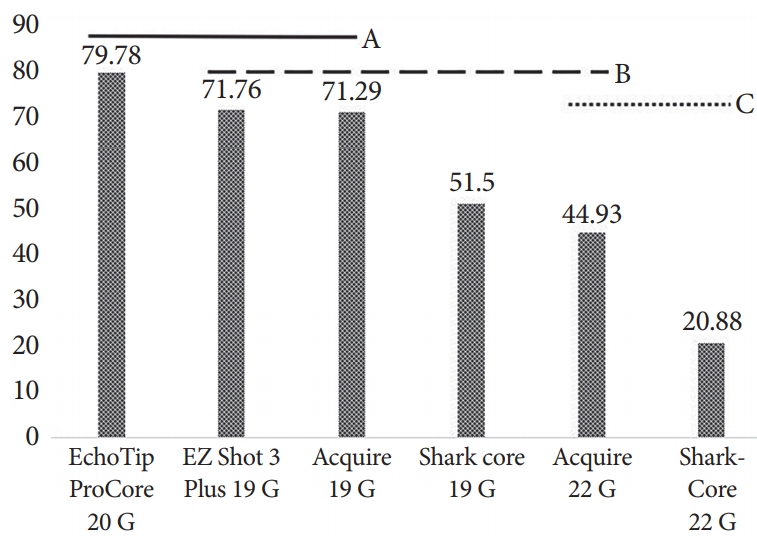
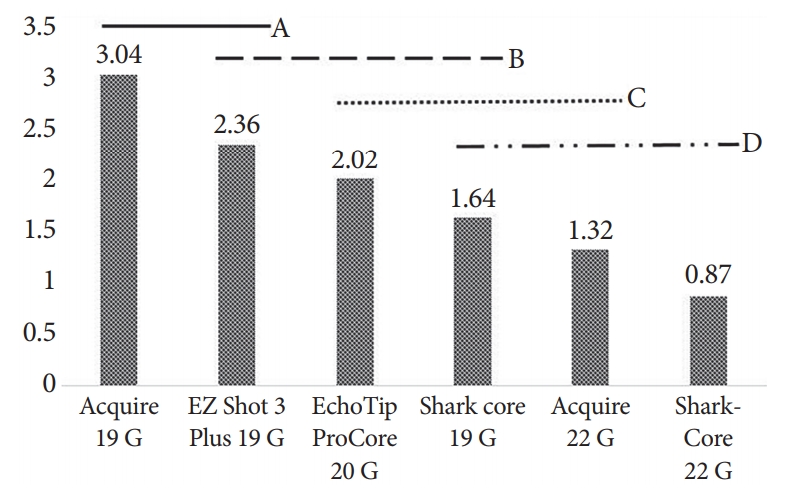
The primary outcome was the number of portal tracts obtained per needle aspirate. A complete portal tract (CPT) was defined as containing all 3 portal structures (portal vein, hepatic artery, and bile duct). Two pathologists who were blinded to the needle type independently reviewed each sample and counted the number of CPTs. The secondary outcomes were the mean specimen fragment length per needle aspirate and the mean total specimen length. Comparisons between needle types for the 3 outcomes (1 primary outcome and 2 secondary outcomes, univariate analysis) were performed using analysis of variance (ANOVA) and TukeyŌĆÖs post-hoc analysis. All possible pairs of means were compared, and all p-values were adjusted for multiplicity. In the graphical representation of the difference in the measured outcomes, the letters (A, B, C, D) indicate groupings where means are not statistically significantly different, with 5% alpha within the same letter.
RESULTS
The performance of the tested needles is summarized in Table 1. The Acquire 19 G needle yielded the highest mean number of CPTs (11.8┬▒4.87), whereas the SharkCore 22 G yielded the lowest (1.4┬▒1.34, p<0.0001). However, as shown in Fig. 3, ANOVA demonstrated that all 19 G and 20 G needles yielded statistically similar mean CPTs. The yields of the larger-bore needles were superior to those of the 22 G SharkCore needle (p<0.0001 for Acquire 19 G, p=0.0005 for EZ Shot 3 Plus 19 G, p=0.0004 for SharkCore 19 G, p=0.02 for EchoTip ProCore 20 G). For the mean total specimen length, the yield of EchoTip ProCore 20 G was the longest and that of SharkCore 22 G was the shortest (79.8┬▒15.9 mm vs. 20.9┬▒11.5 mm, p<0.0001). There was no statistically significant difference in total specimen length among the three 19 G needles and the 20 G needle tested (Fig. 4).
The longest mean fragment length was obtained by Acquire 19 G (3.04┬▒0.27 mm), whereas the shortest fragment was obtained by SharkCore 22 G (0.87┬▒0.380 mm, p<0.0001). The Acquire 19 G needle yielded statistically longer tissue fragments than all the other needle types tested, except for the EZ Shot 3 Plus 19 G needle (Fig. 5). There was no statistically significant difference between the two 22 G needles examined in terms of the number of CPTs, mean fragment length, and mean total specimen length (p=0.07, p=0.59, and p=0.10, respectively).
DISCUSSION
Liver biopsy is commonly the final step in the evaluation of liver disease and is regularly used to objectively measure the degree of liver fibrosis. Recently, EUS has emerged as a useful tool for obtaining liver biopsy specimens, as it provides real-time guidance for the target, including identification of focal lesions as well as of the presence of prominent portal hypertensive vasculature patterns [6,7]. Among several factors that determine the usefulness of a liver biopsy specimen for diagnosis and staging, 2 main variables have been suggested, namely specimen length and number of CPTs. It is generally agreed that the specimen should be at least 15 mm in length and contain 6ŌĆō8 CPTs [8]. In prospective studies on EUS-guided needle biopsy using fine-needle aspiration (FNA) or fine-needle biopsy (FNB) needles, specimen adequacy criteria of 6 or more CPTs and 15 mm specimen length were reached in >90% of the cases [9,10]. As interest in EUS-guided liver biopsy has been growing, newer needle designs have become available to improve the yield of this procedure.
In this ex vivo study, we compared the yields among more comprehensive, recently available 19 G (3), 20 G (1), and 22 G (2) needles with various needle tip geometries, with the number of CPTs as the primary outcome. We found no significant difference among the three 19 G needles and the single 20 G needle for the primary outcome. The performance of some needle designs in liver biopsy has been compared in 2 previous ex vivo studies [11,12]. Lee et al. compared four 19 G FNA needles (Cook EchoTip ProCore, Olympus EZ Shot 2, Boston Scientific Expect Slimline, and Medtronics SharkCore) and one 18 G Tru-Cut percutaneous needle (TruCore; Argon Medical Devices, Frisco, TX, USA) in 2 normal human cadaveric livers [12]. A total of 12 biopsy specimens were taken using each needle, with 3, 6, and 9 actuations in each pass [12]. In the study, the SharkCore 19 G needle yielded significantly higher number of CPTs (mean 8.83) than the other 19 G needles. The 18 G Tru-Cut percutaneous needle yielded 7 CPTs (p>0.05). In comparison, our current study also incorporated the newly employed Franseen-type (Acquire) and Menghini-type (EZ Shot 3 Plus) EUS-FNB needle tip designs in addition to the fork-tip needle (SharkCore). The utilization of the needles with their redesigned tip geometry with improved yield is supported by a recent report on the Franseen vs. fork-tip types of needle in sampling of pancreatic mass lesions [13]. Other potential causes of the variation in results may include the different biopsy techniques and the use of fresh liver specimen in our study, in contrast to the use of a cadaveric liver with potentially different tissue or cellular cohesiveness.
The significance reached in the study by Lee et al. may also be derived from the relatively low number of CPTs obtained by the other (Expect, EchoTip, and EZ shot) 19 G needles, which have the traditional needle-tip design, in comparison to other previous studies [12]. For instance, Diehl et al. used Expect or Expect Flexible needles in 110 human subjects, and reported a median CPT of 14 compared to the reported mean of 4.42 by Lee et al. [10,12] Furthermore, 105 of the 110 patients in the study had >6 CPTs [10]. As for the EchoTip needle, whereas Lee et al. reported a mean CPT of 3.3, Stavropoulos et al. reported a median CPT of 9 with 91% of patients having >6 CPTs [9,12]. As for the SharkCore 19 G needle, we reported a mean CPT of 10.4, which is similar to the 8.8 CPTs reported by Stavropoulos et al. [9]
In another ex vivo study on 2 human cadaveric livers by Schulman et al., three 19 G needle types (SharkCore FNB, Expect FNA [Boston Scientific, Natick, MA, USA], and ProCore FNB [EchoTip HD ProCore]) and one 22 G (SharkCore FNB) needle were compared with 2 percutaneous 18 G (QuickCore [Cook Medical] and Coaxial Temno [Care-Fusion, McGaw Park, IL, USA]) needles for the primary outcome of number of CPTs [11]. In this study, in which a total of 288 biopsy specimens were taken (48 per needle type), the 19 G SharkCore needle outperformed all the other needle types with a mean CPT of 6.2. Additionally, the 22 G SharkCore FNB needle yielded significantly more portal tracts than the Expect FNA (3.8 vs. 1.9, p=0.004), ProCore FNB (3.8 vs. 1.7, p=0.012), and percutaneous 18 G (3.8 vs. 2.5, p=0.05) needles [11]. It is worth mentioning that although the number of CPTs in our work is closer to that reported in previous human studies, the CPTs obtained by the 19 G needles in both the studies by Lee et al. and Schulman et al. were lower than the 19 G needle yields in previous reports on humans [11,12]. The mechanistic explanation for this discrepancy is lacking but this difference may also be related to the use of cadaveric liver and/or differences in the aspiration technique. Table 2 shows a comparison of the current study with previous studies on EUS-guided liver biopsy with non-Tru-Cut needles.
Our study has limitations that merit discussion. We paid attention to using a fresh liver specimen and to the scope positioning to mimic real-life tissue sampling as much as possible. Although this effort enabled obtaining a range of CPT counts close to those obtained in previous in vivo human studies, there may be differences in real-life tissue sampling arising from anatomical and technical variations for each patient and operator. In addition, the use of a bovine specimen in our study might raise concerns; however, it seems reasonable to consider that the performance can be translated to human liver specimens as the bovine liver shares the overall anatomical and physical properties of the human liver [14]. Finally, as we experimented on an ex vivo liver model, adverse events could not be assessed.
In conclusion, the literature is scarce with respect to EUS-guided liver biopsy techniques that yield the optimal specimen for pathological analysis. The available studies considerably vary in needle design and biopsy technique. Our current study provides an initial, but revealing, data demonstrating comparable outcomes with the use of multiple newly designed 19 G needles for liver biopsy. This finding is clinically relevant because it suggests that the endoscopist can choose a needle based on his or her comfort and experience and institutional availability without concerns over diagnostic performance. Further studies may be needed to assess the ease of needle use in various anatomical locations and for confirming the optimal needle design in a larger sample.