INTRODUCTION
Endoscopic ultrasound (EUS)-guided biliary drainage has recently emerged as a common alternative for endoscopic transpapillary drainage.1 In particular, EUS-guided hepaticogastrostomy (EUS-HGS) is widely performed not only as an alternative to transpapillary biliary drainage, but also for primary drainage of malignant biliary obstruction.2 Although several devices and technical tips to maximize the safety of EUS-HGS have been developed, the risks of nonnegligible adverse events, such as bleeding,3 bile peritonitis,4 and stent migration,5 remain. For anatomical reasons, this technique is associated with a risk of mispuncturing the intrahepatic vessels, which might cause death due to massive bleeding.6 Several reports have already investigated the use of EUS-guided coiling for hemostasis of variceal bleeding. However, no cases of EUS guidance after portal vein mispuncture have been reported.7,8 We report a technique for troubleshooting EUS-guided portal vein coiling to prevent bleeding from the intrahepatic portal vein after mispuncture during interventional EUS.
CASE REPORT
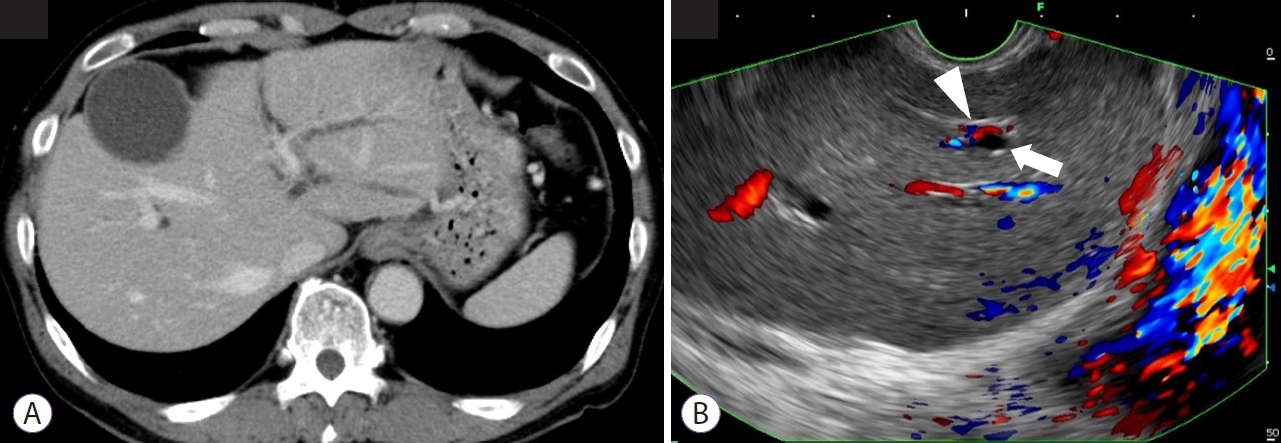
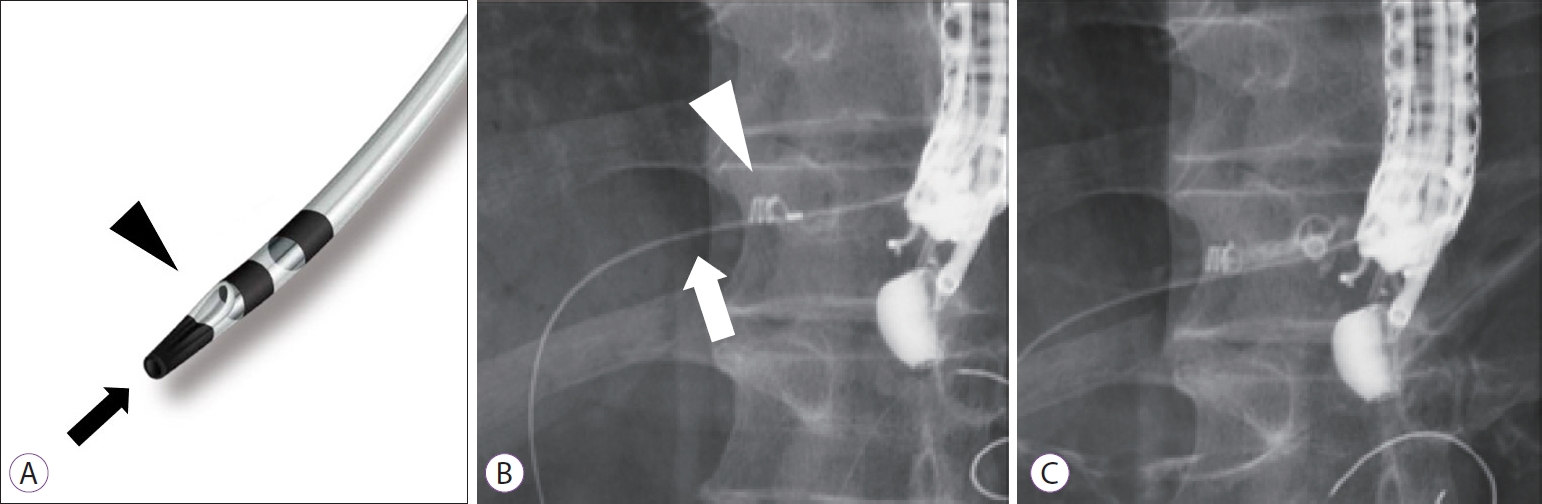
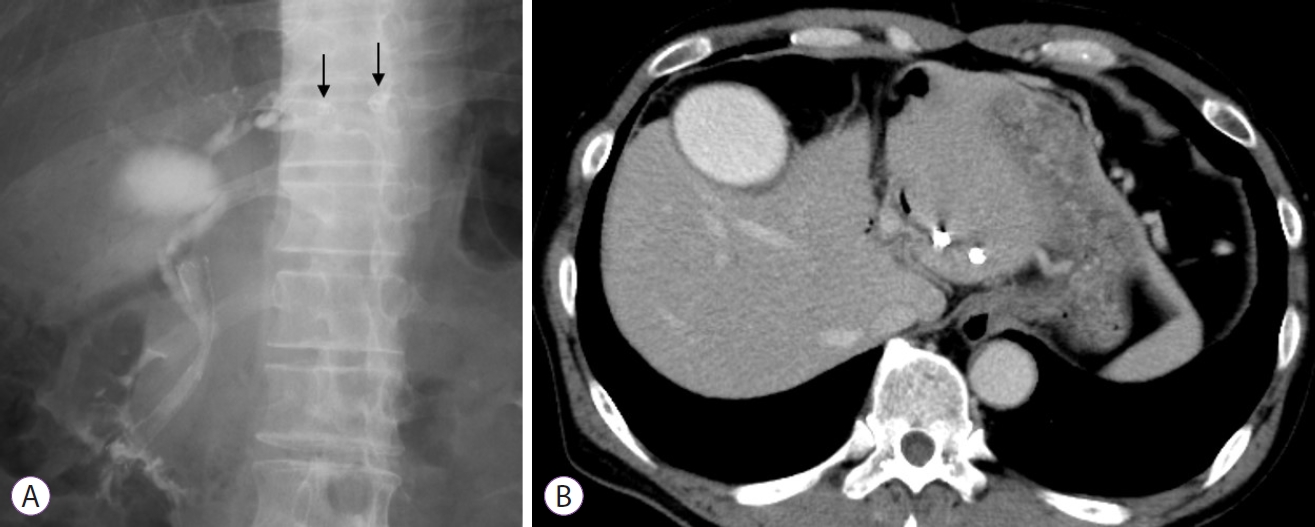
A 59-year-old male patient with unresectable pancreatic cancer was admitted for liver dysfunction during chemotherapy. Computed tomography (CT) revealed distal biliary obstruction due to tumor progression and dilatation of the intra- and extrahepatic bile ducts (Fig. 1A). EUS-HGS was planned because duodenal stenosis due to duodenal invasion was evident on endoscopy. Using an echoendoscope, the intrahepatic bile duct (Fig. 1B) was visualized from the stomach. On EUS, the targeted branch of the bile duct was dilated to 2.8 mm. Branches of the intrahepatic portal vein were visualized close to the bile duct (Fig. 1B). The bile duct was carefully punctured with a 19-gauge needle, and a guidewire was inserted. As the contrast medium injected from the needle seemed to have accumulated in the bile duct, a 7-Fr bougie dilation catheter with a Y-connector attachment was inserted along the wire. After injection of contrast medium through the dilation catheter, we diagnosed catheter mispuncture into a branch of the intrahepatic portal vein, because the contrast medium rapidly disappeared with blood flow. To prevent bleeding from the dilated puncture site of the intrahepatic portal vein, embolization coil placement was planned. Initially, the bougie dilation catheter was replaced with a double-lumen cannula (Uneven Double Lumen Cannula; Piolax Medical Systems, Kanagawa, Japan) (Fig. 2A). A first coil (MReye embolization coil, 3 mm; Cook Japan, Tokyo, Japan) was placed into the periphery of the punctured portal vein (Fig. 2B, C), and a second coil was placed into the liver parenchyma along the puncture route (Fig. 2C). The double-lumen cannula was useful because the coils could be inserted from the side port under stabilization of the cannula with the guidewire through the main port. After the placement of the embolization coils, no bleeding into the abdominal cavity or stomach was observed on EUS or endoscopy. Secure hemostasis was confirmed by EUS with color Doppler imaging. Finally, we managed to place the transpapillary stent (Fig. 3A). Following these procedures, the patient was asymptomatic. CT performed the next day revealed no complications (Fig. 3B).
DISCUSSION
We reported the case of a patient treated with embolization coil placement immediately after mispuncture of an intrahepatic portal vein during EUS-HGS. Procedures for EUS-guided embolization coil placement have mostly been reported for the treatment of bleeding from esophageal or gastric varices.7,8 Another case of EUS-guided coil placement for the treatment of bleeding from a portoduodenal fistula has been reported.9 However, this is the first report of EUS-guided placement of embolization coils to prevent bleeding after EUS-HGS.
Complications of EUS-HGS have recently been recognized after the publication of numerous experiences.1 Bleeding after EUS-HGS was reported in some case reports and original articles, and the occurrence rate was reported as 0% to 8%.1 In most reported cases, the bleeding points are the puncture site or gastric wall and are treated conservatively. Cho et al.10 described a case of bleeding from the intrahepatic portal vein, which was treated by placement of a metal stent in their prospective study. Although bleeding from a portal vein after EUS-HGS has not been reported frequently, bleeding after mispuncture of the portal vein is considered a potential risk, because intrahepatic bile ducts and portal veins usually exist side by side. In general, when a needle is accidentally inserted into an intrahepatic portal vein during biliary drainage procedures such as percutaneous or EUS-guided transhepatic biliary drainage, withdrawing the needle from the mispunctured portal vein into the hepatic parenchyma and maintaining the needle in place for a few minutes until thrombus formation in the portal vein might be sufficient to prevent bleeding.11 These techniques are usually used when percutaneous transhepatic biliary drainage (PTBD) is performed, and bleeding from the portal vein after PTBD does not lead to death in most cases.12 However, more attention should be paid to bleeding when the punctured wall of the portal vein is dilated. In our EUS-HGS procedure, bile duct puncture was confirmed with EUS guidance and fluoroscopic images of contrast medium accumulation. On fluoroscopic imaging, if the contrast medium does not disappear, the bile duct has been punctured correctly. However, during the reported procedure, the targeted intrahepatic bile duct was not greatly dilated (2.8 mm in diameter), and the injected contrast medium from the puncture needle seemed to remain. Therefore, we could not find any mispuncturing of the portal vein. Thus, insertion of the dilation catheter could not be avoided in this case. Furthermore, if the needle had been withdrawn when bleeding occurred after puncturing the portal vein, immediate insertion of coils or other hemostatic materials might have been difficult. Because of these circumstances, placement of embolization coils into the mispunctured portal vein was considered reasonable. Transpapillary drainage was selected after coil placement. As in previously reported case10 where the intrahepatic portal vein was injured during EUS-HGS and a metal stent was placed, stent placement via the hepaticogastrostomy route may help achieve hemostasis. However, it seemed difficult to puncture the same site of the intrahepatic bile duct again and insert the stent after coil placement. If the intrahepatic bile duct that was downstream to the puncture site were targeted, a second puncture and stent placement could be successful. However, if the stent had been placed in the downstream bile duct, the effect of compressing the injured site cannot be predicted. Therefore, we selected this coil-based strategy.
In previously reported procedures for EUS-guided coil placement, coils have mostly been inserted through the puncture needle.7-9 In contrast, a double-lumen cannula was used for coil placement in our procedure. In the treatment of varices, the targets of coil placement are usually dilated vessels, where keeping the needle tip inside the dilated vessel is not particularly difficult. However, with coil placement into the portal vein during EUS-HGS, maintaining the needle tip inside the portal vein is difficult because the portal vein around the bile duct is not usually dilated. To perform our procedure precisely, the tip of the device used for coil insertion must be kept stable inside the portal vein. The double-lumen cannula has two lumens: one is available for a 0.025-inch guidewire, and the other is available for a 0.035-inch guidewire (Fig. 2A). A double-lumen cannula with a guidewire inserted through the main port allowed stabilization of the cannula tip inside the portal vein. The procedure was shown in Supplementary Video 1. In addition, the placement of multiple coils through the side port was facilitated by this method (Fig. 2B, C).
EUS-guided biliary drainage is mostly regarded as an alternative to endoscopic retrograde cholangiopancreatography (ERCP).1 In most published articles, EUS-HGS was performed for patients in whom placement of transpapillary stents failed. However, EUS-HGS was performed prior to the ERCP in the current case. For patients with duodenal stenosis, as occasionally seen with pancreatic cancer, re-intervention for stent dysfunction after transpapillary stenting usually becomes difficult. In contrast, reintervention after EUS-HGS is easily performed if duodenal stenosis is present.2 For these reasons, EUS-HGS prior to transpapillary procedures appears feasible, although transpapillary stenting was finally achieved in the present case.
In summary, we have reported the first case in which the patient was treated with EUS-guided portal vein coiling for troubleshooting a complication of EUS-HGS.