INTRODUCTION
The endoscopic retrograde cholangiopancreatography (ERCP)-related perforation are rare but sometimes carries 16% to 18% of death rate.1 The incidence of perforation has been reported from 0.3% to 2.2%.2-5 ERCP-related perforation is classified into three or four types based on anatomical location and the mechanism of injury.2,3 The management of ERCP-related perforation has been differentiated by the types of perforation. Guidewire perforation are benign and in general do not require surgery.2,3 Periampullary perforations with the diagnosis of retroperitoneal air may be managed nonsurgically such as by aggressive endoscopic drainage and medical treatment with broad spectrum antibiotics.3,5 But patients with retroperitoneal fluid collection have worse prognosis and require surgical intervention.2 Here, we present our experience in a case of ERCP-related severe ampullary perforation with retroperitoneal fluid collection that was treated nonsurgically with a covered metal stent.
CASE REPORT
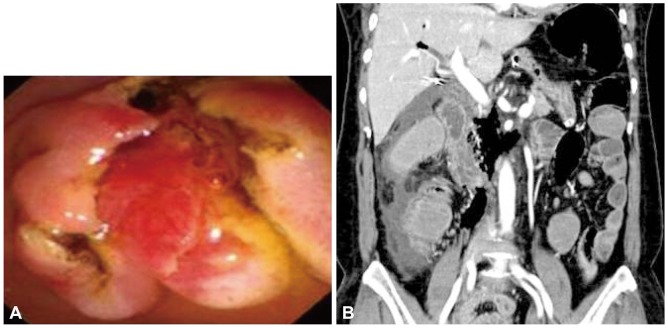
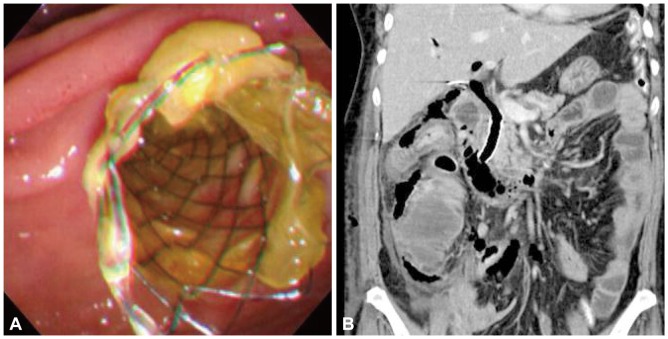
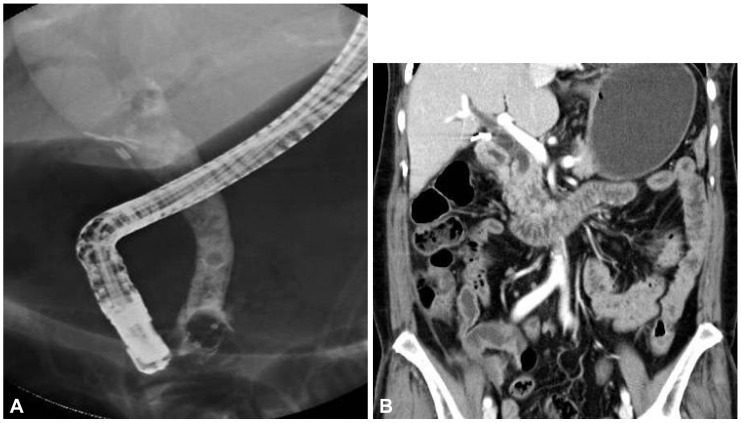
A 61-year-old Korean woman was referred to our hospital for right upper quadrant pain. She had undergone cholecystectomy for acute calculous cholecystitis 4 years ago. Initial abdominal computed tomography (CT) showed biliary tree dilatation but, although periampullary swelling was suspected, no definite occluding lesion was evident. ERCP was performed to obtain a biopsy specimen from the ampulla, which showed nonspecific dilatation of the common bile duct (CBD) without a definite mass around the ampulla. A specimen was taken from the ampulla after endoscopic sphincterotomy (Fig. 1A). The day after the ERCP, she developed a severe right flank pain and fever of 39т, shortness of breath (26/min), and rapid pulse rate (102/min). A physical examination revealed decreased bowel sound and whole abdominal distension. CBC showed intense leukocytosis (22,000/mm3) and neutrophila (94.6%). Arterial gas analysis showed hypoxemia (pO2=60.8 mm Hg on room air). Abdominal CT revealed retroperitoneal air and fluid collection suggesting post-ERCP ampullary perforation (Fig. 1B). Although her symptoms were severe, her condition looked stable and there was no sign of sepsis, and conservative treatment was considered. Subsequent ERCP revealed ampullary edema only, but the cholangiography showed continuous leakage of the radiocontrast media from the ampullary level. Although the perforating point was not visualized, a 5-cm long, 10-mm in diameter, full-covered metal stent (Niti-s; Taewoong Medical, Seoul, Korea) was inserted to seal the perforation defect and to provide a lumen for biliary drainage (Fig. 2).The fever and the abdominal pain after the ERCP subsided at day 4 after the stenting. She was fasted for 6 days and intravenous antibiotics and fluids were administered. Her clinical course was uneventful. Oral feeding was resumed at day 7 after the stenting. No further surgical intervention was necessary. Retroperitoneal air and fluid collection gradually resolved by follow-up abdominal CT and thus the stent was extracted at day 10 (Fig. 3A). The patient was discharged on day 23 after ERCP and consequent abdominal CT revealed complete resolution of the retroperitoneal fluid collection (Fig. 3B).
DISCUSSION
Traditionally, traumatic periduodenal perforation has been managed surgically. The recent paradigm of management, however, has shifted to a more selective approach that requires consideration of perforation type and surgical indications.2,3,6 The majority of patients without free wall duodenal perforation or peritoneal signs are being treated nonsurgically.2,4,7 The retroperitoneal air is a common finding indicating nonsurgical management and the amount of retroperitoneal air is not correlated with clinical course. For those treated conservatively, biliary drainage is the mainstay of treatment to reduce morbidity and mortality3 and is usually consisted of endoscopic nasobiliary drainage (ENBD) and endoscopic retrograde biliary drainage (ERBD). The finding of retroperitoneal fluid collection, however, suggests continued bile leak from the site of perforation. It is suggested that patients with retroperitoneal fluid collection have worse prognosis and require surgical intervention.2,6
However, the traditional drainage methods such as ENBD or ERBD may be limited for preventing bile and pancreatic fluid leakage, especially when severe CBD dilatation or a large perforation hole is present. Surgery should be undertaken, therefore, if pain and abdominal signs are prominent, if suppuration is suspected, or if symptoms do not improve after a brief period of nonoperative management.8
Biliary self-expanding metal stents have the advantage of being inserted with small sizes and provide large diameters for biliary drainage; however, their use in benign conditions has been limited, mainly because of difficulty in extracting them. On the other hand, a covered stent has been occasionally used to treat an esophagorespiratory fistula or an esophageal rupture.9 In cases of ampullary perforation, a covered stent can provide complete sealing of the perforation defect and the stent lumen may allow physiologic drainage of bile and thus prevent additional fluid leakage. A small sized report suggested that fully covered metal stents were removed without any complication after being placed in the CBD for a mean time of over 4 months and that it could be used in the management of benign biliary conditions.10
Recently, a case of persistent duodenal fistula caused by sphincterotomy-related duodenal perforation was reported. The patient underwent an ERCP and sphincterotomy, after which a retroperitoneal duodenal perforation occurred. She underwent a laparotomy and drainage of the retroperitoneal space. After that, a high volume duodenal fistula developed. However, the fistula healed completely after the transient use of stents.11 Based on this concept, we applied a covered stent to the perforation site immediately after the perforation developed, and achieved complete resolution of the retroperitoneal fluid collection and rapid clinical improvement. However, despite this treatment success, the merits of covered stents for ampullary perforation with retroperitoneal fluid collection have not been fully established because nonsurgical treatment failures have a high complication rate, with a potentially fatal outcome. Therefore, management using a covered stent and serial follow-up by abdominal CT may be useful treatment option for ERCP-related ampullary perforation with retroperitoneal fluid collection in selected patients.