INTRODUCTION
Esophageal endoscopic submucosal dissection (ESD) is widely performed for early stage neoplasms of the esophagus [1]. With various innovations such as submucosal injection [2] and traction methods [3], ESD can now be performed safely. Patients with esophageal carcinoma usually have a history of excessive alcohol consumption. Thus, sedation with benzodiazepines can occasionally cause disinhibition during an ESD, which may render the procedure more difficult and unsafe. For this reason, general anesthesia has recently been used for esophageal ESD. ESD under general anesthesia is suitable and safe [4], however, some peculiar complications such as a sore throat due to intubation, malignant hyperthermia, and hypothermia occur during ESD under anesthesia. Herein, we report a case of perforation of a gastric tear during an esophageal ESD under general anesthesia.
CASE REPORT
A 68-year-old woman with esophageal squamous cell carcinoma was referred to our institution after the tumor was detected during a routine esophagogastroduodenoscopy (EGD). Although she did not take any medications, she had a history of excessive alcohol consumption. On magnifying endoscopy with narrow band imaging and endoscopic ultrasonography, the lesion was located within the mucosal layer in the upper esophagus. Thus, for removal, ESD was scheduled and was started under general anesthesia with desflurane, propofol, and remifentanil hydrochloride. Rocuronium bromide was also administered as a muscle relaxant.
ESD was performed conventionally using carbon dioxide insufflation. Preoperative EGD showed no gastric atrophy in this case.
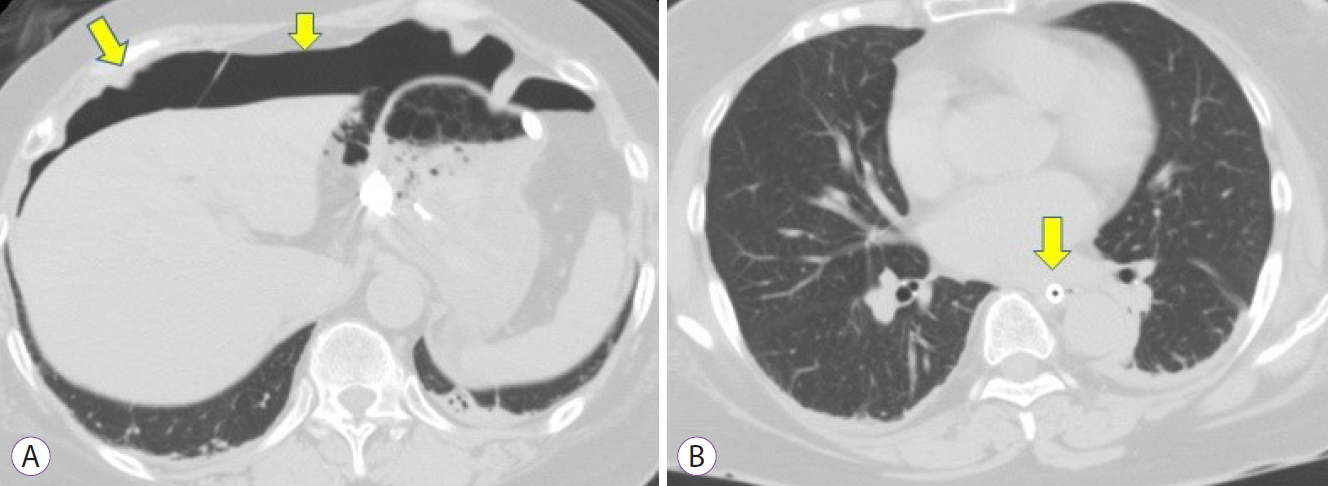
When an endoscope was advanced into the stomach for suction of the liquid and the air during the dissection, gastric tears were observed without any evidence of perforation or bleeding. Complete resection was achieved after 44 min, and the size of the resected specimen was 25├Ś24 mm, and the size of the lesion was 13 ├Ś8 mm. After retrieving the specimen, the endoscope was reinserted into the stomach to confirm the tears. Detailed observation revealed multiple gastric tears, one of which was bleeding, with a perforation in the lesser curvature of the gastric upper body and fornix. The perforation site was immediately closed endoscopically using endoclips (Fig. 1). Computed tomography was performed to evaluate the perforation, which revealed free air in the peritoneum and retroperitoneum. Free air was considered to be caused by the gastric perforation because there was no perforation or injury to the muscle layer in the ESD site (Fig. 2), and pneumomediastinum and subcutaneous emphysema were not observed (Fig. 3).
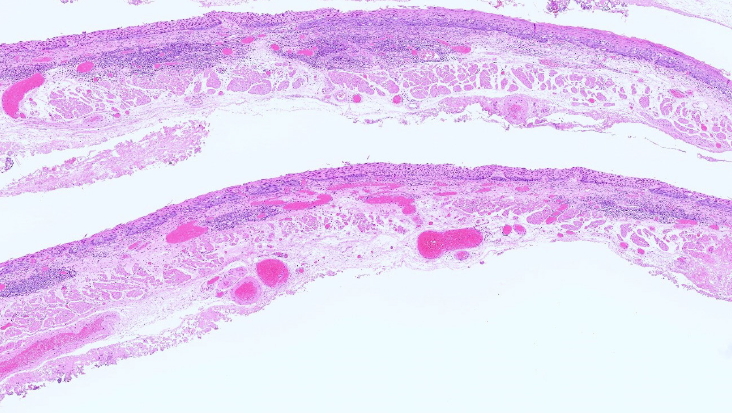
The patient was treated conservatively with intravenous antibiotics (1 g cefazolin, twice daily for 7 days). Moreover, she started drinking water and began a diet on the 5th and 6th days post-ESD, respectively. The histology of the resected lesion revealed a squamous cell carcinoma limited to the intraepithelial layer with no evidence of the resected muscle layer (Fig. 4). The patient was discharged on the 8th postoperative day without any sequelae.
DISCUSSION
Mallory-Weiss tears (MWT) occur rarely as a complication of ESD, with an incidence of 0.07ŌĆō0.49% [5]. Iatrogenic tears usually occur in the atrophic stomach, mostly in the right lateral wall of the esophagus and the lesser curvature of the gastric upper body [6]. In our case, multiple lacerations also occurred at the lesser curvature of the gastric upper body and fornix. Chen et al. [7] reported 20 cases (5.4%) of MWT detected during an esophageal ESD under general anesthesia, with only one case of MWT perforation. In addition, female sex and procedure time longer than 88.5 min were shown to be independent risk factors (odds ratio=5.270 and 3.953, respectively) for MWT during esophageal ESD. Although the sex of our patient was female, the procedure time was not long.
Since esophageal ESD requires a precise technique and has a high complication rate, reliable sedation is needed to perform an esophageal ESD. Conscious sedation is suitable for endoscopic procedures. However, since alcohol consumption which causes inadequate sedation, including disinhibition, is the most important risk factor for esophageal squamous cell carcinoma, conventional sedation may be insufficient for esophageal ESD [8]. The usefulness of general anesthesia has been reported for esophageal ESD [4,9]. General anesthesia has peculiar complications, including our case.
Esophageal ESD tends to cause gastric inflation because gas suction in the esophagus does not effectively reduce the gas in the stomach. This necessitates repeated suction of the gas in the stomach during an esophageal ESD. Gastric inflation under general anesthesia will not only cause discomfort to the patients but will also lessen the diaphragmatic movement and reduce the tidal volume of ventilation. General anesthesia may also induce gastric inflation due to diminished tonus of the gastric muscles. Additionally, less belching under general anesthesia can also cause an increase in the volume of the gastric gas.
Carbon dioxide, due to its rapid absorption, is useful to avoid gas-related complications, compared to air [10]. Although the severity of complications such as perforation and pneumomediastinum are diminished by the use of carbon dioxide, it does not contribute to the prevention of MWT caused by gastric inflation. This is because its absorption in the stomach and intestine is rapid but not instantaneous. Therefore, both monitoring of the volume of the gastric gas and a frequent gas suction are important to reduce gas-induced complications during esophageal ESD.
In conclusion, although general anesthesia is useful for esophageal ESD, MWT induced by gastric overinflation under general anesthesia is a complication that cannot be ignored. The frequent suction of gastric gas during the procedure may diminish this type of complication.