An Impacted Pancreatic Stone in the Papilla Induced Acute Obstructive Cholangitis in a Patient with Chronic Pancreatitis
Article information
Abstract
Obstructive jaundice is very rarely caused by impaction of a pancreatic stone in the papilla. We report here on a case of obstructive jaundice with acute cholangitis that was caused by an impacted pancreatic stone in the papilla in a patient with chronic pancreatitis. A 48-year-old man presented with acute obstructive cholangitis. Abdominal computed tomography with the reconstructed image revealed distal biliary obstruction that was caused by a pancreatic stone in the pancreatic head, and there was also pancreatic ductal dilatation and parenchymal atrophy of the pancreatic body and tail with multiple calcifications. Emergency duodenoscopy revealed an impacted pancreatic stone in the papilla. Precut papillotomy using a needle knife was performed, followed by removal of the pancreatic stone using grasping forceps. After additional sphincterotomy, a large amount of dark-greenish bile juice gushed out. The patient rapidly improved and he has remained well.
INTRODUCTION
Chronic pancreatitis is an inflammatory disease that is characterized by progressive destruction of the pancreatic parenchyma and fibrosis of the ductal structures. It is often complicated by the formation of pancreatic stones within the main pancreatic duct or by obstructive jaundice due to the biliary stricture. Obstructive jaundice caused by impaction of a pancreatic stone in the papilla is very rare in a patient with chronic pancreatitis.1-6
Endoscopic therapy for chronic pancreatitis can decrease or resolve the need for surgical procedures, and it may serve as a bridge therapy to surgery for non-operative candidates, and it can also help predict the response to surgical therapy.7 In general, the aim of endoscopic therapy in patients with painful chronic pancreatitis with a dilated pancreatic duct is to relieve the outflow obstruction of the pancreatic duct or the common bile duct, and to extract the stones.
We report here a case of obstructive jaundice with acute cholangitis, which was caused by an impacted pancreatic stone in the papilla of a patient with chronic pancreatitis. The impacted pancreatic stone was successfully extracted with a precut papillotomy.
CASE REPORT
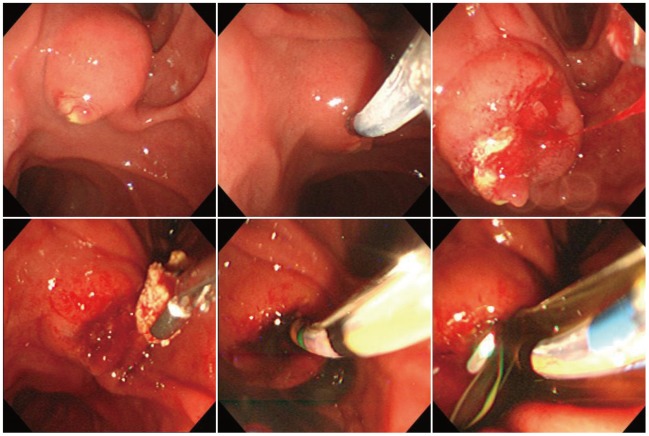
A 48-year-old man presented with acute obstructive cholangitis. He had previously been admitted several times for alcohol-induced chronic pancreatitis with acute exacerbation. His laboratory test revealed white blood cell count of 12,250/mm3, aspartate aminotransferase level of 83 U/L (normal, 0 to 40 U/L), alanine aminotransferase level of 160 U/L (normal, 0 to 40 U/L), alkaline phosphatase level of 919 U/L (normal, 40 to 250 U/L), total bilirubin level of 4.19 mg/dL (normal, 0.2 to 1.2 mg/dL), direct bilirubin level of 3.52 mg/dL (normal, 0.05 to 0.5 mg/dL), amylase level of 182 U/L (normal, 20 to 125 U/L) and lipase level of 127 U/L (normal, 13 to 60 U/L). Abdominal computed tomographic (CT) scanning with the reconstructed image revealed distal biliary obstruction that was caused by a pancreatic stone in the pancreatic head, and there was also pancreatic ductal dilatation and parenchymal atrophy of the pancreatic body and tail with multiple calcifications (Fig. 1). The diameter of the stone in the pancreatic head was measured to be about 1 cm. Compared with the previous CT taken 3 years ago (Fig. 2), the multiple pancreatic calcifications were further increased. Emergency duodenoscopy revealed swelling of the papilla and an impacted pancreatic stone in the papilla (Fig. 3). Precut papillotomy using a needle knife (Huibregtse; Cook Medical, Winston-Salem, NC, USA) was performed without preceding biliary cannulation. The precut incision was extended to the roof of the papilla in a 12 o'clock direction, and a whitish-yellow stone was exposed. The pancreatic stone was successfully removed using grasping forceps (Rat Tooth; Olympus, Tokyo, Japan). After additional sphincterotomy with a pull-type papillotome (Tri-Tome PC; Cook Medical), a large amount of dark-greenish bile juice gushed out. The rest of the stones in the pancreatic duct were not removed. The patient has rapidly improved after the endoscopic therapy and he has remained well since then.

Abdominal computed tomographic scanning with the reconstructed image revealed distal biliary obstruction by pancreatic stone in the pancreatic head, pancreatic ductal dilatation and parenchymal atrophy of the pancreatic body and tail with multiple calcifications. The diameter of the impacted stone in the pancreatic head was measured to be about 1 cm.
DISCUSSION
The complications of chronic pancreatitis are commonly associated with obstructive jaundice or pancreatic stones. The generally known mechanism for obstructive jaundice is the stenosis of the bile duct occurring as a consequence of recurrent acute inflammatory episodes, which may ultimately result in periductal fibrotic stricture.8-11 Stenosis of the bile duct occurs more commonly in patients with advanced chronic pancreatitis, with the highest incidence in the calcific variant. Stenosis of the bile duct occurs in up to 30% of the patients with chronic pancreatitis, 28% of them complicated by obstructive jaundice or cholangitis, and these cases require treatment, including surgical procedures or endoscopic intervention.8-11 But obstructive jaundice caused by the impaction of a pancreatic stone in the papilla in a patient with chronic pancreatitis is very rare, with only eight cases having been reported to date.1-6
The mechanism of the obstructive jaundice caused by pancreatic stones may be similar to that of gall stone pancreatitis.6 Impaction of pancreatic stones in the main pancreatic duct near the papilla results in obstruction of the bile duct, leading to obstructive jaundice and acute cholangitis.6 In general, gall stone pancreatitis is considered to be mainly caused by relatively small stones. But in a previous report, the pancreatic stones causing impaction in the papilla were relatively larger than the biliary stones, measuring about 7 to 20 mm.6
Endoscopic retrograde cholagiopancreatography for the evaluation and treatment of symptomatic pancreatic duct stones in patients with chronic pancreatitis provides direct assessment and restores important functions of the pancreatic duct. Because of the reduced invasiveness of endoscopic procedures compared with that of surgery, endoscopic procedures may be preferred and surgery is reserved as a second-line therapy for patients in whom endoscopic therapy has failed or is ineffective.12 For the patients with painful chronic pancreatitis and a dilated pancreatic duct, endoscopic treatment consisting of the drainage of the main pancreatic duct, extraction of stones or drainage of a pseudocyst is used increasingly with a high degree of technical success and good clinical results.7 If the pancreatic stones are large and impacted, extracorporeal shock wave lithotripsy is required to be performed before endoscopic removal can be achieved.13
Obstructive jaundice caused by the impaction of pancreatic stones in the papilla has previously been treated successfully by the endoscopic therapy.6 The endoscopic methods include endoscopic sphincterotomy, endoscopic pancreatic sphincterotomy and precut papillotomy using a needle knife. In patients in whom the insertion of a papillotome is impossible due to the impaction of the pancreatic stone in the papilla, the precut papillotomy using a needle knife is useful and effective, because it allows improvement of the jaundice and removal of the stones at the same time and the procedure is effective for decreasing the risk of papillary re-impaction.6
To the best of our knowledge, this is a very unusual and rare case of acute obstructive cholangitis caused by an impacted pancreatic stone in the papilla. We think performing precut papillotomy using a needle knife is useful for treating this condition.
Notes
The authors have no financial conflicts of interest.