INTRODUCTION
Gastric inverted hyperplastic polyp (IHP) is a rare type of gastric polyp and is marked by downward growth of hyperplastic mucosal component into the submucosa. Generally, gastric hyperplastic polyps grow upward to the lumen of the stomach, but gastric IHP grows downward into the submucosa. Therefore, the polyp is formed in the submucosa. The polyp is composed of foveolar-type cells, pyloric gland-like cells, and smooth muscle cells. In 1993, Kamata et al.1 termed the lesion inverted hyperplastic polyp. As far as we know, one case has been reported previously in Korea.2 A total of six cases of gastric IHP coexisting with gastric adenocarcinoma have been reported in the world.3
Here, we report a case of gastric IHP coexisted with metachronous early gastric cancer managed successfully by the endoscopic submucosal dissection.
CASE REPORT
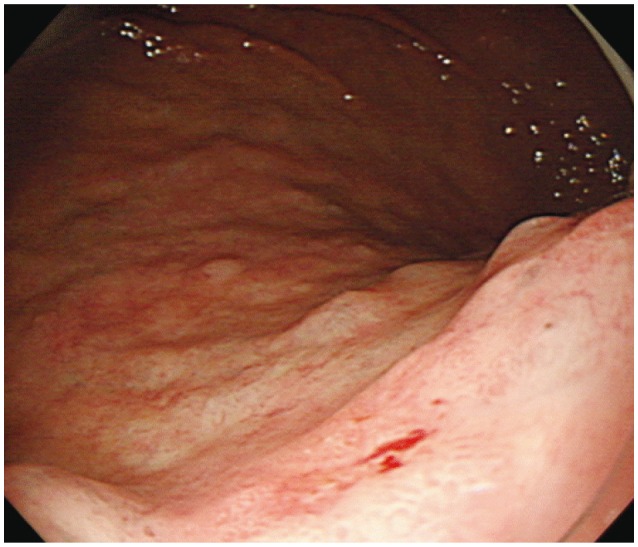
A 77-year-old male was admitted to undergo gastric endoscopic submucosal dissection. He had been diagnosed with a metachronous early gastric cancer on the posterior wall of the mid body 2 weeks before the admission. In the past history, he had undergone endoscopic submucosal dissection due to early gastric cancer on the anterior wall of the antrum of the stomach and gastric polypectomy due to multiple hyperplastic polyps in the stomach 1 year and 8 months before the admission. On admission, the physical examination was unremarkable. Complete blood count results showed white blood cell of 5,800/mm3, hemoglobin of 13.1 g/dL, and platelet of 214,000/mm3. The blood chemistry was analyzed as total protein of 7.6 g/dL, albumin of 4.1 g/dL, total bilirubin of 0.6 mg/dL, aspartate aminotransferase of 33 IU/L, alanine aminotransferase of 23 IU/L, alkaline phosphatase of 51 IU/L, serum creatinine of 1.4 mg/dL, total cholesterol of 176 mg/dL, and fasting blood glucose of 97 mg/dL. Endoscopic examination demonstrated superficial depressed lesion with spontaneous bleeding on the posterior wall of the mid body (Fig. 1). He underwent endoscopic submucosal dissection successfully.
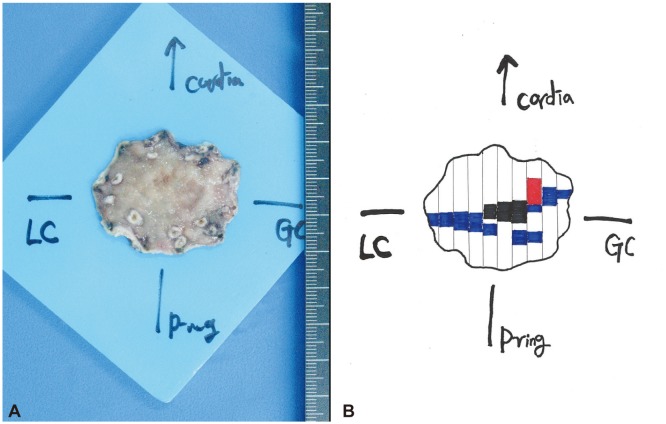
The resected specimen was 4.5У3У0.5 cm and had 1.5У0.5-cm superficial depressed lesion in the center (Fig. 2). Microscopically, 1.5У0.5-cm-sized, well-differentiated tubular adenocarcinoma was noted. It was confined to the mucosa and did not have involvement of lateral and deep margins, lymphatic invasion, vascular invasion, and perineural invasion. In addition, gastritis cystica profunda was also noted in the submucosa. Especially, nodular inverted proliferation of the normal appearing gastric epithelium and glands in the submucosa was noted in the center of the resected specimen. It measured 5 mm and showed mild glandular atypia. It was diagnosed to be a gastric IHP (Fig. 3). He was discharged without special complications after the endoscopic submucosal dissection.
DISCUSSION
Gastric IHP is characterized by marked submucosal glandular proliferation associated with cystic dilation, leading to a polypoid lesion. The main location is the submucosa or the inside of the muscularis mucosae. Similar lesions arising in the colon have been reported as colonic IHP.4 Colonic IHP differs clinically from exophytic hyperplastic polyps by being more frequent on the right side than in the left colon and being relatively more common in women. Colonic IHP, coexisting with colitis cystica, relates to colonic malignancy.4
In Kono et al.'s report3 analyzing 32 gastric IHP cases (in 30 patients), the mean age was 55.6 years (range, 8 to 81), consisting of 14 male and 16 female patients. Fifteen of the 32 gastric IHPs were located in the fundus, 12 in the body, and five in the antrum of the stomach. The size of the lesion varied and six of the 32 IHPs were greater than 3 cm in diameter. The glandular components of gastric IHP comprised fundic type epithelium in 13 cases, and foveolar-type epithelium and pylorictype epithelium or another intermediate-type epithelium in the remaining 19 cases. Gastritis cystica profunda in the background of the stomach has been reported in only two cases.
In our case, gastric IHP was located in the body and showed foveolar-type epithelium and pyloric-type epithelium. One notable feature of our case was accompanying adenocarcinoma in the mucosa. According to Kono et al.'s report,3 six of the reported 30 patients had synchronous gastric cancer. The adenocarcinoma developed separately from the IHP in five patients. But the adenocarcinoma developed from IHP itself in only one patient. As gastric IHP is very rare, the relation between gastric IHP and adenocarcinoma has not been known until now. However, the frequency is considerably higher compared with the incidence of gastric carcinoma occurring in the general population. Therefore, it may be necessary to evaluate the presence of adenocarcinoma in IHP patients.
In our case, gastritis cystica profunda was also noted in the submucosa. Gastritis cystica profunda (GCP) is an uncommon hyperplastic benign lesion, and histologically characterized by hyperplasia and cystic dilatation of the gastric glands extending into the submucosal layer. GCP usually occurs at a gastroenterostomy site, although it can occasionally be found in an unoperated stomach. GCP is considered to be a benign disease, but it is thought to be a possible precancerous lesion, since a few gastric cancers were reported to be associated with it.5-9 Both IHP and GCP are located in the submucosa and are composed of benign glandular components associated with cystic dilatation. IHP revealed hyperplastic glands composed of epithelium of foveolar-type cells, pyloric gland-like cells, and smooth muscle cells. On the other hand, GCP is usually composed of simple, glandular components without hyperplastic changes.10 If there is a submucosal glandular displacement, it may be difficult to distinguish between IHP and GCP. Although Yamashita et al.11 proposed the possibility that IHP may be associated with hyperplastic changes of GCP, further studies are necessary to clarify the association between IHP and GCP.
We reported a case of gastric IHP associated with GCP and EGC. Therefore, precise endoscopic examination may be necessary to rule out gastric malignancy in IHP patients.