Esophageal Involvement of Pemphigus Vulgaris Associated with Upper Gastrointestinal Bleeding
Article information
Abstract
Esophageal involvement of pemphigus vulgaris is rare, and when present, the most common presenting symptoms reported in the medical literature are odynophagia and dysphagia. Here, we present two cases of pemphigus vulgaris presenting with upper gastrointestinal hemorrhage because of esophageal involvement of the disease. In case 1, a 41-year-old female patient with a prior diagnosis of pemphigus vulgaris presented with hematemesis. Esophagogastroduodenoscopy showed diffuse mucosal exfoliation and oozing bleeding of the oropharynx and esophagus. The patient recovered after the administration of high-dose corticosteroids and immunosuppressants. In case 2, a 30-year-old female patient with known pemphigus vulgaris also presented with hematemesis, showing similar endoscopic findings to the first case. She also responded to the same treatment. Esophageal involvement of pemphigus vulgaris responds to high-dose corticosteroids and immunosuppressants. Thus, in patients with pemphigus vulgaris with signs or symptoms of upper gastrointestinal bleeding, an early endoscopy for the evaluation of esophageal involvement is beneficial.
INTRODUCTION
Pemphigus vulgaris (PV) is a rare autoimmune blistering disease involving the skin and mucosa. In PV, mucosal lesions usually develop in the oral and pharyngeal areas.1 The involvement of the esophagus is rare;2,3 however, some authors suggest that it may be more prevalent than expected. When involvement of the esophagus is present in PV, the most common presenting symptoms are dysphagia and odynophagia. In one prior study of esophageal PV, dysphagia, and odynophagia was present in 57.1% and 21.4% of the patients, respectively, whereas hematemesis was present in only 3.5%.4 Here, we present two cases with PV with initial symptoms of hematemesis.
CASE REPORTS
Case 1
A 41-year-old female patient presented to our hospital emergency center with the chief complaint of hematemesis that developed 2 hours ago (total amount, >1 L). PV had been pathologically confirmed in this patient 5 years ago through skin biopsy. Her skin lesions had recurrently aggravated with the discontinuation of corticosteroids, and thus she had been on maintenance therapy for >3 years (oral methylprednisolone 10 mg daily and mycophenolate mofetil [MMF] 500 mg twice daily). She had no other medical history.
On physical examination, her initial blood pressure was 90/60 mm Hg, pulse rate was 97 beats per minute, respiratory rate was 20 breaths per minute, and body temperature was 37.5℃. She showed multiple scars on the face and upper chest due to the healing of earlier skin involvement of PV; however, she did not show any active bullae or desquamation. The baseline laboratory results were as follows: hemoglobin level, 10.7 g/dL; white blood cell count, 19,010/µL; and platelet count, 479,000/µL. The serum levels of routine chemistry markers were within the reference limits.
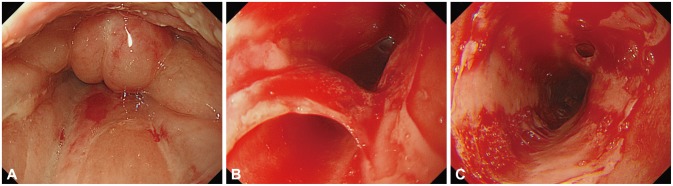
Initial esophagogastroduodenoscopy showed severe mucosal edema and erythema on the oropharynx and laryngeal area, with desquamation (Fig. 1A). From the upper esophageal sphincter to the lower esophagus, there was diffuse exfoliation of the mucosa with multiple linear ulcerations and erosions (Fig. 1B). There was no current active bleeding; however, subepithelial hemorrhage was present, with the friable mucosa bleeding easily on touching (Fig. 1C). The gastric mucosa and duodenal mucosa were well preserved without signs of hemorrhage or mucosal breakage. Because of the concern of additional bleeding risk, esophageal biopsy was not done. Immediately after the endoscopy was done, the patient experienced dyspnea and her oxygen saturation dropped to 88% on pulse oximetry monitoring, owing to severe laryngeal edema. She shortly recovered completely in a few minutes after supplementation with oxygen and administration of 100 mg intravenous hydrocortisone. Thereafter, she was maintained on intravenous hydrocortisone 100 mg twice daily for 6 days, and did not show any signs or symptoms of gastrointestinal bleeding or airway obstruction. After diet build-up and switching to oral methylprednisolone 16 mg daily with MMF 500 mg twice daily, she was discharged on the 11th day of hospitalization. We recommended a follow-up evaluation of esophagogastroduodenoscopy for pathologic confirmation of the diagnosis; however, the patient refused. She is currently in remission status on MMF 500 mg twice daily and methylprednisolone 8 mg daily, without recurrent hematemesis.
Case 2
A 30-year-old female patient was referred to our hospital emergency center with hematemesis that started several hours before her presentation. The hematemesis had a total amount of 500 mL, had the color of fresh blood, and was combined with sloughed tissue material. PV had been diagnosed in this patient 11 months previously. Two weeks previously, her dermatologist had decided to increase the quantity of her medication because of new formation of vesicles on her skin. After switching from oral methylprednisolone 2 mg daily, cyclosporine 50 mg twice daily, and MMF 1,000 mg twice daily to oral methylprednisolone 4 mg daily, cyclosporine 150 mg twice daily, and MMF 1,000 mg twice daily, the skin lesions had shown improvement at the time of admission.
On physical examination, her initial blood pressure was 140/90 mm Hg, pulse rate was 118 beats per minute, respiratory rate was 20 breaths per minute, and body temperature was 36.5℃. She did not show any newly or recently developed skin lesions but had chronic scars due to PV on the trunk, inguinal, and perioral skin areas. The baseline laboratory results were as follows: hemoglobin level, 10.0 g/dL; white blood cell count, 16,940/µL; and platelet count, 262,000/µL. The serum levels of routine chemistry markers were within the reference limits.
Initial esophagogastroduodenoscopy results revealed multiple mucosal abrasions in the oral cavity (Fig. 2A), with combined laryngeal edema (Fig. 2B). In the upper esophagus, there was a longitudinal ulceration covered with exudate, and diffuse mucosal friability and erythema that was consistent with the findings of exfoliative esophagitis (Fig. 2C). There was no abnormality in the lower esophagus, stomach, and duodenum. After the administration of intravenous hydrocortisone 100 mg twice daily for 2 days, the patient did not show any other symptoms, and we were able to rapidly taper off the corticosteroids. On the third day of hospitalization, she underwent a follow-up esophagogastroduodenoscopy, which showed markedly improved mucosal exfoliative lesions in the oral cavity (Fig. 3A) and upper esophagus (Fig. 3B), for which biopsy was done. The final pathology report indicated detached squamous epithelium, with acute and chronic inflammation and necroinflammatory exudates. She was discharged on the sixth day of hospitalization with MMF 1,000 mg twice daily. Thereafter, she was referred back to a local clinic, and has not returned to our center.

Endoscopic findings. (A) Mucosal abrasions on the oral cavity wall. (B) Erythematous mucosa with severe edema of the larynx. (C) Linear ulceration in the esophagus covered with exudate.
DISCUSSION
Esophageal involvement of autoimmune blistering skin diseases is a rare condition that, even when present, may be underrecognized or misdiagnosed without a proper endoscopic evaluation.5,6
In our two cases, esophageal involvement of PV presented with a large amount of upper gastrointestinal bleeding. Both patients showed severe laryngeal edema, which can lead to desaturation and dyspnea, as in case 1. On endoscopic evaluation in both cases, mucosal lesions were found in the oropharynx, with exfoliative esophagitis.
We successfully treated both patients with early administration of systemic corticosteroids and immunosuppressive therapy after confirming the diagnosis of esophageal involvement of PV. As most patients with PV are frequently maintained on oral corticosteroid therapy, which is a risk factor for peptic ulcer disease that may lead to ulcer bleeding, the possibility of peptic ulcer should be ruled out before additional corticosteroid administration. The recognition of esophageal involvement is important, as early management with corticosteroids and immunosuppressive therapy may improve the clinical outcome. Thus, in patients with PV or other autoimmune blistering skin diseases, early endoscopic evaluation may be indicated when signs or symptoms of esophageal involvement are present.7
Notes
The authors have no financial conflicts of interest.