INTRODUCTION
Early detection of gastric cancer is difficult even among well-trained endoscopists, leading to frequently missed lesions [1]. Although the accurate diagnosis and growth characteristics of gastrointestinal lesions are well described because of the development of magnifying and image-enhanced endoscopy, the usefulness of early detection through screening remains unclear. Recently, a new laser endoscopic system has been developed, which includes linked color imaging (LCI) and blue laser imaging (BLI), which are receiving a great deal of attention for the early detection of gastrointestinal cancers [2,3]. LCI provides color information regarding the red, green and blue components and provides an expanded color range, which causes red and white colors to become redder and whiter, respectively [2,4,5]. LCI facilitates easier recognition of even small differences in mucosal color, although the mucosal colors obtained by LCI are similar to those obtained using white light imaging. BLI provides color information regarding the green and blue components and provides high color contrast between malignant lesions and the surrounding mucosa, in near and close-up views [6,7].
Endoscopists may occasionally face difficulties with identifying gastric lesions, particularly those located on the posterior gastric wall and/or near the gastric angle. The degree of difficulty varies depending upon the various kinds of endoscopes used. A few gastric cancers are difficult to identify in tangential views using a normal-caliber endoscope under direct vision, resulting in missed lesions. A small-caliber endoscope has a small radius at the tip of the endoscope, which allows observation of upper gastrointestinal lesions in a frontal view [8]. Small-caliber endoscopy has been reported to provide poor quality endoscopic images compared with normal caliber endoscopy [9-11]. However, recent progress with the development of improved technology can deliver high-resolution images. LCI and BLI with a small-caliber endoscope (EG-L580NW; Fujifilm, Tokyo, Japan) using a laser endoscopic system have been available since 2014. However, whether LCI and BLI using a small-caliber endoscope can yield findings similar to normal-caliber endoscopy for gastrointestinal lesions remains undetermined, although it is commonly used in Japan to screen for upper gastrointestinal lesions.
We report a patient with an early gastric cancer of the posterior wall near the gastric angle, which was difficult to diagnose using only white light imaging, as well as a normal-caliber endoscope at the time of screening. BLI with a small-caliber endoscope was used in this patient.
CASE REPORT
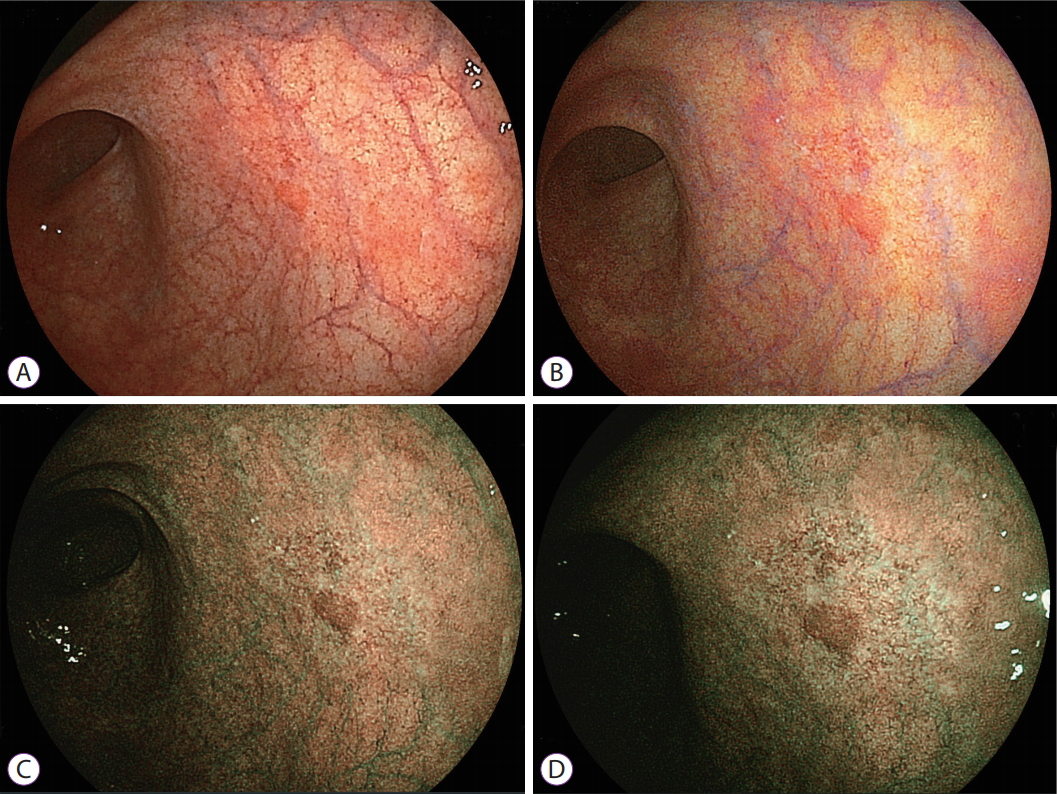
A 79-year-old man underwent esophagogastroduodenoscopy with a small-caliber endoscope (EG-L580NW; Fujifilm) using a laser endoscopic system as part of a medical examination at a Neurology clinic. He complained of slight epigastric bloating. He reported a history of hypertension and was prescribed an antihypertensive drug. He reported no other symptoms at the time of the esophagogastroduodenoscopy. Laboratory tests showed anti-Helicobacter pylori antibody 6.4 IU (positive) and a positive stool antigen test for H. pylori. Other blood and chemistry tests showed normal results. Abdominal ultrasonography and a computed tomography scan showed no abnormal findings. White light imaging with a small-caliber endoscope showed a red area measuring 3 mm in diameter on the posterior gastric wall near the gastric angle (Fig. 1A), which was not suspicious for gastric cancer based on its appearance. LCI enhanced the red lesion and the surrounding red area (Fig. 1B). BLI revealed a discolored lesion measuring 10 mm around a central red area with an apparent demarcation between the cancer and the surrounding mucosa with high color contrast (Fig. 1C, D). Several irregular vessels were observed on the discolored lesion even with the use of small-caliber endoscopy, suggesting an early gastric cancer. The biopsy showed well-moderately differentiated tubular adenocarcinoma. The patient was referred to Jichi Medical University Hospital for further evaluation and treatment.
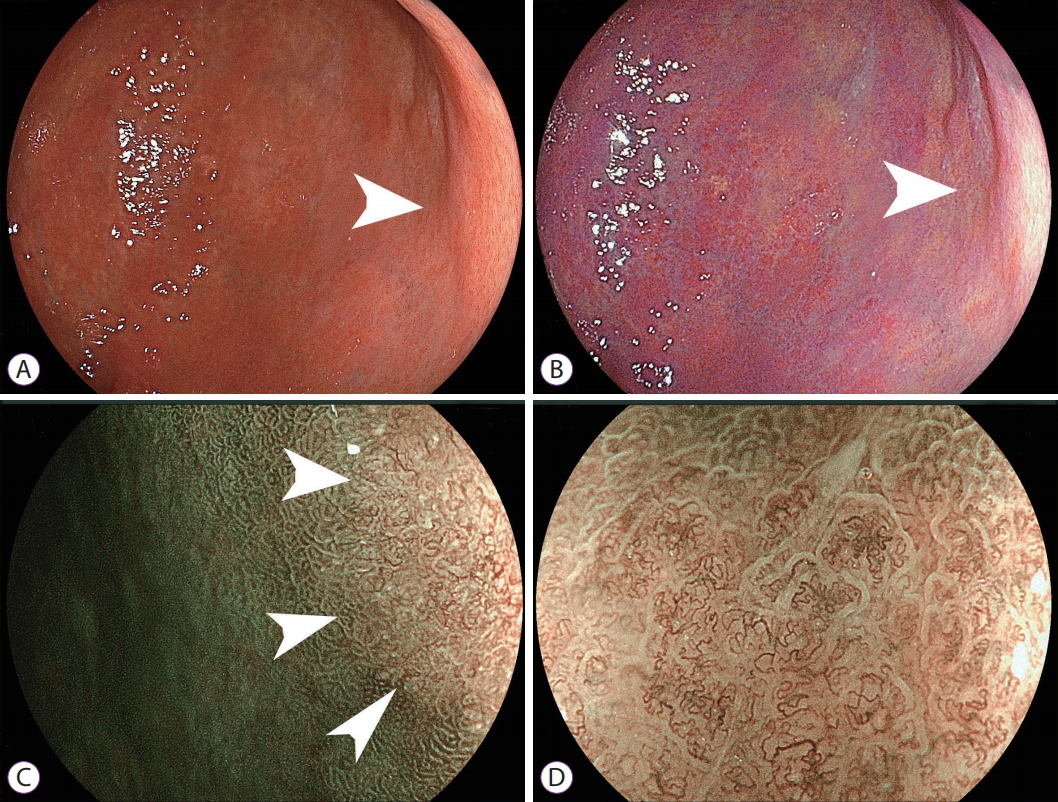
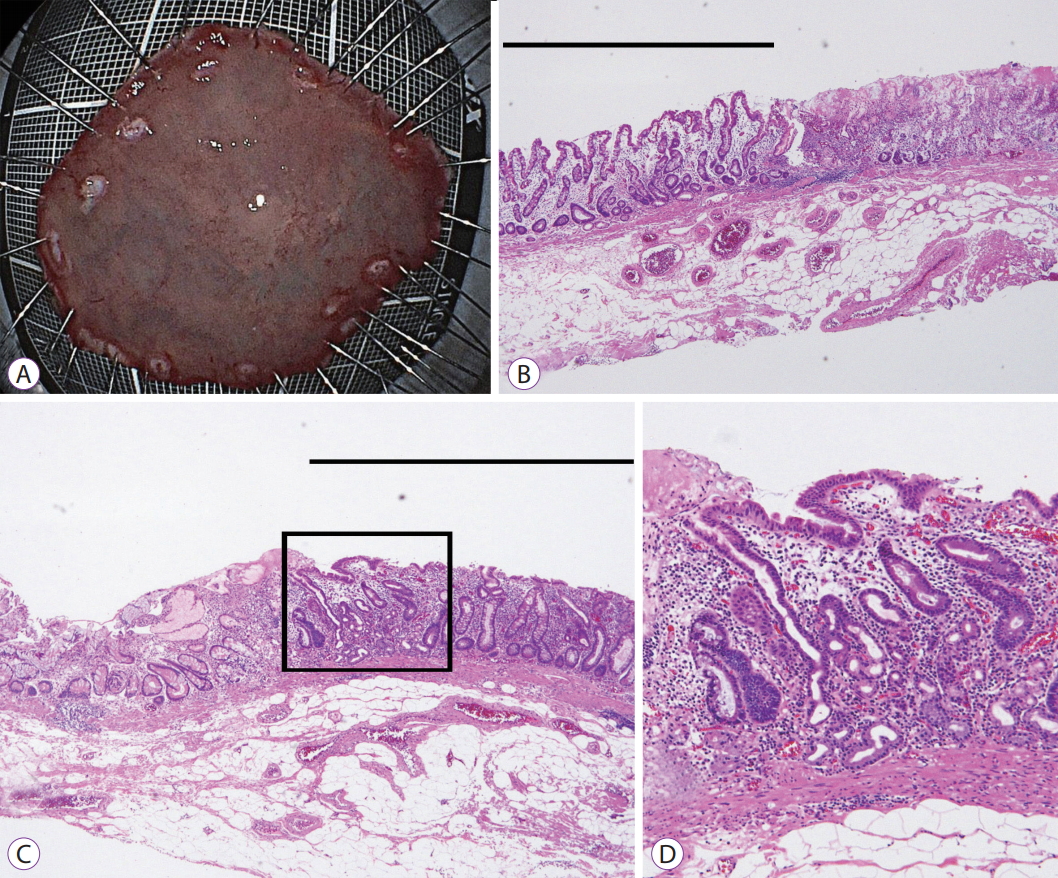
Laser endoscopy was performed using a transoral endoscope (EG-L590ZW; Fujifilm); however, the lesion could not be clearly visualized without magnification because of tangential views obtained (Fig. 2A, B). Magnified BLI imaging showed an apparent demarcation between the slightly depressed cancer and the surrounding mucosa, as well as irregular microvessels and microstructure distinct from the surrounding mucosa (Fig. 2C, D). Endoscopic ultrasound revealed cancer limited to the mucosa. Two months later, marks were placed 5 mm outside the demarcation line, and endoscopic submucosal dissection was performed (Fig. 3A). The resected specimen showed a slightly depressed early gastric cancer with well-moderately differentiated tubular adenocarcinoma limited to the mucosa (Fig. 3B, C). Additionally, microvessels were identified in the intervening part of the superficial layer of the mucosa (Fig. 3D), supporting the identification of vessels with BLI using small-caliber endoscopy.
DISCUSSION
BLI performed with a small-caliber endoscope allows detection of features of early gastric cancer that are difficult to detect using white light imaging. Although white light imaging showed only a small red area, BLI showed a larger discolored lesion around it with irregular vessels suspicious for early gastric cancer. Additionally, this endoscope allowed us to observe the lesion under direct vision despite its location on the posterior wall near the gastric angle. Small-caliber endoscopy using BLI provided accurate and clear images, even during routine health examination.
It is difficult for many endoscopists to recognize the subtle color changes in the gastric mucosa as a definitive cancer [12]. Most gastric cancers are surrounded by chronically inflamed mucosa with atrophic changes and intestinal metaplasia [13-15]. These surrounding features make it difficult to identify the demarcation between a malignant lesion and the surrounding mucosa. Recently, laser endoscopy has been developed and is reported to be useful for the diagnosis of a few gastrointestinal lesions [3,16-20], although to date, no studies have reported using small-caliber laser endoscopy.
In this patient, BLI allowed detection of an early gastric cancer with a clearly apparent demarcation, which could not be observed using white light imaging. Many endoscopists in Japan use a small-caliber endoscope to screen patients for upper gastrointestinal lesions. The endoscope with a diameter measuring 5.9 mm causes minimal pain and gag reflex during the endoscopic examination. Using the laser endoscopic system, small-caliber endoscopy produces bright and high-resolution white light images that are suitable for screening patients for upper gastrointestinal lesions. However, in this patient, white light imaging did not reveal definitive findings of gastric cancer. Most areas of cancer showed a color similar to the surrounding mucosa using white light imaging, whereas BLI showed a different color. During screening examinations, endoscopists must not depend only on conventional color patterns using white light imaging to avoid missing upper gastrointestinal lesions. Large differences in color between malignant lesions and the surrounding mucosa lead us to evaluate suspicious areas more carefully. Recently, LCI has been used to screen patients for early gastric cancers [2,5] and showed an enhanced malignant lesion in this case as well. Additionally, the results of this case report suggest that BLI may also be suitable to identify early gastric cancers in a few areas of the stomach such as antrum or near angle where brighter images are not required.
Small-caliber laser endoscopes have a short focal length of 3 mm and thus allow close-up views. Laser endoscopy produces a combined image created using spectral and white light imaging. BLI has a high emission intensity at 410 nm (short wavelength) reflecting on the mucosal surface in addition to low intensity white light imaging. These characteristics may be useful to enhance the visibility of details on the tumor surface, even with small-caliber endoscopy. In this patient, using BLI, an irregular vascular pattern was visualized in the malignant portion but not in the surrounding mucosa. The small radius of the endoscope tip enables endoscopists to observe lesions near the gastric angle under direct vision. A normal-caliber endoscope may occasionally not show lesions in this area because of an inappropriate distance between the lesion and the tip of the endoscope. These characteristics of small-caliber endoscopy also help to distinguish malignant from non-malignant lesions.
This report describes the usefulness of LCI and BLI with a small-caliber endoscope to establish the diagnosis of an early gastric carcinoma. A large prospective controlled trial is warranted to demonstrate the usefulness of BLI with a small-caliber endoscope for the diagnosis of early gastric cancer. In conclusion, white light imaging using small-caliber endoscopy may not allow the diagnosis of a small red lesion as cancer; however, BLI could show a discolored area around the lesion with irregular vessels distinct from the surrounding non-malignant area, allowing the accurate diagnosis of an early gastric cancer.