See commentary "Endoscopic Management of Acute Cholecystitis Following Metal Stent Placement for Malignant Biliary Strictures: A View from the Inside Looking in" in Volume 52 on page 209 AbstractBackground/AimsIt is often difficult to manage acute cholecystitis after metal stent (MS) placement in unresectable malignant biliary strictures. The aim of this study was to evaluate the feasibility of endoscopic ultrasonography-guided gallbladder drainage (EUS-GBD) for acute cholecystitis.
MethodsThe clinical outcomes of 10 patients who underwent EUS-GBD for acute cholecystitis after MS placement between January 2011 and August 2018 were retrospectively evaluated. The procedural outcomes of percutaneous transhepatic gallbladder drainage (PTGBD) with tube placement (n=11 cases) and aspiration (PTGBA) (n=27 cases) during the study period were evaluated as a reference.
ResultsThe technical success and clinical effectiveness rates of EUS-GBD were 90% (9/10) and 89% (8/9), respectively. Severe bile leakage that required surgical treatment occurred in one case. Acute cholecystitis recurred after stent dislocation in 38% (3/8) of the cases. Both PTGBD and PTGBA were technically successful in all cases without severe adverse events and clinically effective in 91% and 63% of the cases, respectively.
ConclusionsEUS-GBD after MS placement was a feasible option for treating acute cholecystitis. However, it was a rescue technique following the established percutaneous intervention in the current setting because of the immature technical methodology, including dedicated devices, which need further development.
INTRODUCTIONEndoscopic metal stent (MS) placement for malignant biliary obstruction, which has been commonly performed as the standard palliative technique, often causes occlusion of the cystic duct, resulting in acute obstructive cholecystitis at an incidence rate of 5% [1]. Although acute cholecystitis due to gall stones is generally treated with surgical cholecystectomy [2,3], invasive interventions should be avoided when patients have unresectable (i.e., severely progressed) malignant diseases. For palliation of cholecystitis in such patients, percutaneous drainage has long been the sole solution. Although percutaneous transhepatic gallbladder drainage (PTGBD) is a relatively easy technique and has certain efficacy [4], it is related to a lower quality of life (QOL) owing to maintenance of the external drainage tube via the skin. In addition, cholecystitis might recur after catheter removal. Although endoscopic transpapillary gallbladder drainage is an alternative, it can be extremely difficult to perform when an MS has previously been placed in the bile duct.
Since endoscopic ultrasonography (EUS)-guided drainage was first reported in 2001 [5], it has become technically established and improved. Although successful cases of EUS-guided gallbladder drainage (EUS-GBD) have recently been reported at an accelerating pace since Baron et al. first reported it in 2007 [6-23], its efficacy and safety have not been fully established with sufficient accumulation of cases because indications for this technique have been limited to exceptional situations at present. Acute cholecystitis due to obstruction of the cystic duct by an MS in a malignant biliary stricture seems to be an exceptional situation because other interventions, including surgery and PTGBD, have crucial disadvantages [11,16].
In addition, there have been several reports demonstrating lumen-apposing metal stents (LAMSs) as an ideal device for EUS-GBD in comparison with plastic stents (PSs) and traditional MSs. However, LAMSs are not commonly used for EUS-GBD because they are off-label in most countries. Clinical outcomes, including feasibility and long-term outcomes, of EUS-GBD without LAMSs have been extremely scarce, although practitioners must perform EUS-GBD in consideration with such. We retrospectively evaluated EUS-GBD cases and reported the results herein.
MATERIALS AND METHODSPatientsFrom January 2011 to August 2018, 593 patients underwent endoscopic MS placement for unresectable malignant biliary strictures at Sendai City Medical Center. Among them, 10 patients who underwent EUS-GBD for obstructive cholecystitis after MS placement were included in this study. Technical success, clinical effectiveness, procedure-related adverse events, and recurrence of acute cholecystitis were evaluated.
During the defined study period, PTGBD was considered to be the standard intervention for such patients at our center. Percutaneous transhepatic gallbladder aspiration (PTGBA) was attempted when it was thought that obstructive cholecystitis would improve without tube placement in the cases without findings of severe cholecystitis, especially of perforation, pericholecystic/liver abscess, or emphysematous/gangrenous cholecystitis. EUS-GBD was attempted when cholecystitis had not improved with other interventions, when the patient desired to undergo the procedure after signing an informed consent form containing information on the risks and benefits of all treatment options, and when other options were considered to be extremely risky owing to several reasons, such as accompanying dementia or non-cooperation.
For reference, the outcomes of 11 PTGBD procedures and 27 PTGBA procedures that were performed as the initial intervention during the same study period were evaluated (PTGBD/PTGBA as the second intervention after other failed interventions was not included). Since most EUS-GBD procedures were performed on patients who had undergone clinically failed PTGBA, the number of EUS-GBD procedures was counted with an overlap. Owing to the overlap, comparisons between the groups were not performed with statistical analyses.
ProceduresEUS-GBDUsing an echoendoscope (GF-UCT260; Olympus Co., Tokyo, Japan), the gallbladder was visualized from the duodenum or stomach. A 19-gauge needle for EUS-guided fine needle aspiration (Expect, slim line, flex type; Boston Scientific Japan K.K., Tokyo, Japan; or EZShot3 Plus, Olympus Co.) was inserted to the gallbladder. After verification of successful insertion via bile aspiration, a contrast agent was injected to identify the gallbladder fluoroscopically. Along an inserted guidewire, the punctured tract was dilated using a 7-Fr bougie dilator (ES Dilator; Zeon Medical Co., Tokyo, Japan). A cautery dilator (Cyst-Gastro-Set, 7 Fr; Century Medical, Inc., Tokyo, Japan) or a balloon dilator (Ren, 4 mm in diameter; Kaneka Co., Yokohama, Japan) was additionally used when required. Thereafter, a double-pigtail PS (7 or 8 Fr; Gadelius Medical Co., Ltd., Tokyo, Japan) or a fully covered MS (X-Suit NIR, 10 mm in diameter, 4 or 6 cm in length; Olympus Co., WallFlex, 10 mm in diameter, 6 cm in length; Boston Scientific Japan K.K.) was deployed to bridge the gallbladder and gastrointestinal tract. The length of the MS was determined in relation to the size and shape of the gallbladder, puncture site, and distance between the gallbladder and gastrointestinal wall, which increases during the dilation procedure. LAMSs, which were not commercially available in Japan during the study period, were not used in this study.
PTGBDPTGBD was defined as percutaneous drainage with placement of an external tube. Under ultrasonographic guidance, an 18-gauge needle was inserted to the gallbladder via the skin, an intracostal space, and the liver. After verification of successful puncture by aspirating bile and injecting a contrast agent, a guidewire was inserted to the gallbladder. After dilation of the punctured tract using a 7-Fr bougie dilator (Cook Medical Japan, Tokyo, Japan), a 6.5-Fr pigtail catheter (Gadelius Medical Co., Ltd.) was deployed.
PTGBAPTGBA was defined as percutaneous aspiration without tube placement. The gallbladder was punctured using an 18- or 21-gauge needle in the same manner as in PTGBD. After verification of successful insertion by aspirating bile, the infected bile was fully aspirated. When the contents were not sufficiently removed, sterile saline was repeatedly injected, followed by aspiration. Finally, the needle was removed.
DefinitionsAcute cholecystitis was diagnosed in accordance with the Tokyo Guidelines 2007 or 2013 [3]. When diagnosis according to the guidelines was difficult (e.g., in cases with other infectious diseases, a lower conscious level, or a low sensation of pain), it was judged via imaging examinations and/or by using bile cultures. Clinical data were retrospectively collected from the medical records. To describe the general status of the patients, the Charlson Comorbidity Index and the Eastern Cooperative Oncology Group scale were employed [24-26]. The severity of acute cholecystitis was evaluated in accordance with the Tokyo Guidelines 2013.
Technical success was defined as the successful placement of a transluminal stent for EUS-GBD, successful placement of a percutaneous catheter for PTGBD, and successful aspiration of bile during PTGBA. Clinical effectiveness was defined as disappearance of abdominal pain due to cholecystitis with improvement in inflammatory findings, such as body temperature, white blood cell count, and serum C-reactive protein concentration. Procedure-related adverse events were defined as clinically important unfavorable events that occurred within 1 week after the procedure, including bile peritonitis, bleeding, and dislocation of the placed stent or catheter. Bile peritonitis was defined as abdominal pain exacerbated after the procedure. Acute cholecystitis was defined as recurring if it reappeared at least 1 week after the relief of the initial cholecystitis.
The overall survival period after each procedure was calculated using the Kaplan-Meier method. For this analysis, only the last procedure performed on each patient was included (the survival period after the initial procedure was not evaluated for patients who underwent additional procedures owing to clinical failure or recurrence).
RESULTSThe baseline demographics are shown in Table 1. EUSGBD was technically successful in nine cases (Table 2). A PS was deployed in four patients, whereas an MS was used in six patients. Bile peritonitis occurred in four patients after EUSGBD. Among them, two with MSs and one with a PS recovered with conservative treatment. However, one patient who had severe necrotized cholecystitis developed severe peritonitis despite having undergone an unimpeded procedure with a fully covered MS. Emergency surgery was required to remove leaked bile, clean the abdominal cavity with saline, close the hole at the gastric wall created by the EUS-GBD procedure, and perform cholecystectomy. Procedure-related death or other adverse events did not occur.
Acute cholecystitis recurred in three cases (3/8, 38%) within 1 month after the procedure (19, 22, and 22 days). In all patients with recurrent cholecystitis, stent dislocation caused stent dysfunction, which was endoscopically treated by adding a stent via the previously created fistula. A Kaplan-Meier curve of the cumulative stent patency is shown in Fig. 1.
The technical success rate was 100% for the PTGBA and PTGBD groups (Table 3). The clinical effectiveness rate was 91% (10/11) for the PTGBD group and 63% (17/27) for the PTGBA group. Of the 10 patients without clinical response in the PTGBA group, eight underwent EUS-GBD; one underwent surgical cholecystectomy; and the remaining underwent additional PTGBA. Although no clinically important procedure-related adverse events were observed after PTGBD and PTGBA, the placed PTGBD catheter was not removed from one patient until death because it passed through the thoracic cavity owing to the risk of pneumothorax after catheter removal. The PTGBD catheter was removed from the nine remaining patients after recovery from cholecystitis, with an average time of 26 days (range, 15ā56). Among the 10 patients for whom the PTGBD procedure had been clinically effective, acute cholecystitis recurred in one patient 37 days after the procedure (1/10, 10%), which was successfully treated by performing PTGBA. Recurrence after successful PTGBA was observed in three cases (3/17, 18%) 9, 13, and 27 days after the procedure.
The median overall survival period after the last intervention was 217, 178, and 188 days in the EUS-GBD, PTGBD, and PTGBA groups, respectively (Fig. 2).
DISCUSSIONEUS-GBD is an excellent treatment option for acute cholecystitis after MS placement at a malignant biliary stricture because of its low invasiveness in comparison with surgery and better QOL in comparison with PTGBD with external tube placement. Previous studies have reported reasonable outcomes with high technical and clinical success rates. However, in most of the reports (6 out of 11 reports as shown in Table 4), LAMSs, which have not been approved in most countries, have been used [11-23]. Although outcomes with devices that are possibly ideal should be established, outcomes with devices used by common practitioners in the actual clinical setting must be evaluated as soon as possible.
In this study, the technical success and clinical effectiveness rates of EUS-GBD without LAMSs were similar to those in previous reports. However, the adverse event and recurrence rates were relatively high. Several factors seemed to have caused these unfavorable outcomes.
The first factor is the stent selection. Several systematic reviews on stent design have reported that adverse events occur with the use of an LAMS (9.9%), a traditional MS (7.5%ā12.3%), and a PS (15%ā18.2%) in an increasing frequency [27,28]. Conversely, modified self-expandable metallic stents (SEMSs), such as an SEMS with anti-migratory fins and an SEMS with large uncovered flares at both edges, have been reported to be useful with adverse event rates of 0% and 4.8%, respectively [10,12]. LAMSs or MSs modified for EUS-GBD appear safer and should be employed if available.
Second, technical countermeasures may have reduced the adverse events. In most recurrence cases, the stents migrated toward the gallbladder, causing the luminal-side edge of the stent to embed. In all cases, puncture was performed via the stomach, which could drastically move the two punctured points at the gallbladder, and the gastric walls could separate. If the proximal edge located in the stomach is deployed with a sufficient length, such migration can be avoided. Takagi et al. have proposed a modified technique wherein a double-pigtail PS is added to a deployed MS with favorable outcomes, including no stent migration and no recurrence in 16 reported cases [13]. Therefore, routine placement of a double-pigtail PS inside the MS appears favorable if LAMSs cannot be used. When the puncture point is in the stomach, a sufficiently long MS should be used, or a double-pigtail PS deployed in the MS should be fixed to the MS using a clip and/or thread to avoid migration.
Finally, the unfavorable outcomes may have been affected by the patientsā background. This study focused on cases involving not only unresectable malignant biliary strictures, but also acute cholecystitis after MS placement. In the study by Choi et al., a similar adverse event rate of 28.5% under similar conditions has been reported [16]. Highly advanced malignancy and active acute cholecystitis with gallbladder swelling would cause technical difficulty and increase the risk for bile leakage.
The outcomes of the percutaneous intervention in this study were similar to those reported in previous studies [3,4,29,30]. Although the clinical efficacy of PTGBD was found to be acceptable, serious adverse events occurred in some cases [4,31]. In addition, PTGBD requires external drainage, which decreases the QOL in patients with non-curative, advanced malignancy. Even if the tube could be removed, the time to removal is needed, and there is a risk of recurrence. Conversely, PTGBA does not require maintenance of external tubes; however, its clinical effectiveness is limited. Considering the prognoses of patients with end-stage cancer and simplicity of the PTGBA procedure, PTGBA can be performed before EUS-GBD.
For gallbladder drainage after MS placement in the bile duct, a step-up strategy, in which PTGBA is attempted as the first step, possibly followed by EUS-GBD or PTGBD in failed cases, may be acceptable. PTGBA, which was deemed to be sufficiently safe, would be the most reasonable first option in debilitated patients with poor prognoses. In the case of ineffective PTGBA or recurrence after PTGBA, EUS-GBD may be appropriate because constant drainage is possible (unlike PTGBA), with no need for external tubes (unlike PTGBD).
The present study has some limitations owing to its retrospective design and small sample size. However, as EUSGBD does not have priority over percutaneous approaches at present, it should be performed in certain exceptional settings, e.g., in cases where palliation with percutaneous interventions would have excessive risks of accidental withdrawal of the tube owing to confusion. After confirmation of the efficacy and safety in a small population, as in the present study, larger studies are warranted.
In conclusion, EUS-GBD without LAMSs for acute cholecystitis after MS placement for malignant biliary obstruction was found to be a reasonable treatment option in most patients, although adverse events occurred with relatively high frequencies. Therefore, at present, the application of this new technique, when LAMSs and other dedicated stents are unavailable, should be limited to patients who desire the procedure after signing an informed consent form containing information on the risks and benefits of all treatment options, cases in which other intervention has been technically or clinically unsuccessful, and cases in which percutaneous drainage is unfavorable because of accompanying dementia or non-cooperation. Further development of dedicated devices for EUSGBD or approval of LAMSs would improve the outcomes of this procedure. Moreover, further accumulation of cases and prospective studies are necessary.
In conclusion, EUS-GBD without LAMSs for acute cholecystitis after MS placement for malignant biliary obstruction was found to be a reasonable treatment option in most patients, although adverse events occurred with relatively high frequencies. Therefore, at present, the application of this new technique, when LAMSs and other dedicated stents are unavailable, should be limited to patients who desire the procedure after signing an informed consent form containing information on the risks and benefits of all treatment options, cases in which other intervention has been technically or clinically unsuccessful, and cases in which percutaneous drainage is unfavorable because of accompanying dementia or non-cooperation. Further development of dedicated devices for EUSGBD or approval of LAMSs would improve the outcomes of this procedure. Moreover, further accumulation of cases and prospective studies are necessary.
Fig.Ā 1.Kaplan-Meier curve of the cumulative rate of cases without recurrence of acute cholecystitis after endoscopic ultrasonography-guided gallbladder drainage. The mean time to recurrence was 252 days (95% confidence interval, 63ā375 days). 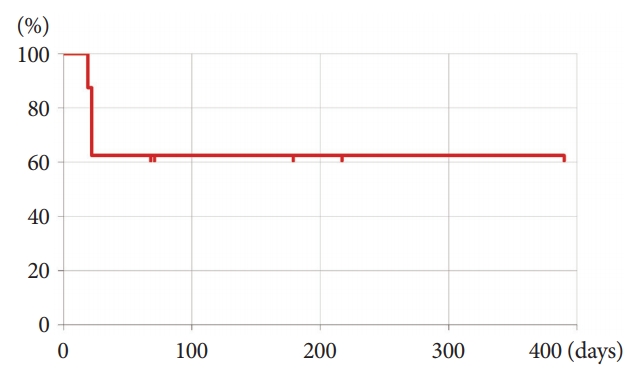
Fig.Ā 2.Overall survival period after the effective intervention for acute cholecystitis. The median survival period was 270 days (95% confidence interval [CI], 72ā362 days) after endoscopic ultrasonography-guided gallbladder drainage (EUS-GBD), 178 days (95% CI, 97ā259 days) after percutaneous transhepatic gallbladder drainage (PTGBD), and 188 days (95% CI, 107ā269 days) after percutaneous transhepatic gallbladder aspiration (PTGBA). 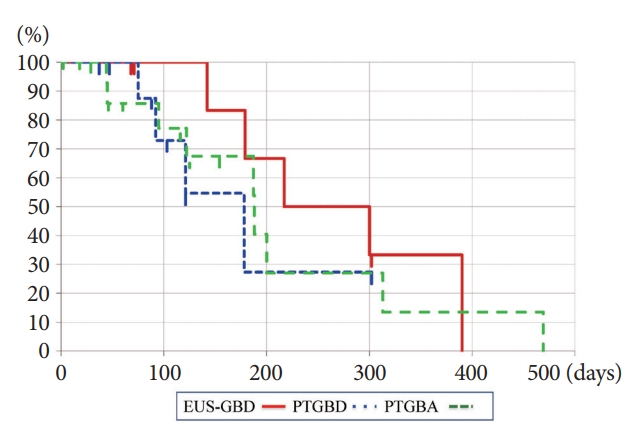
TableĀ 1.Patient Characteristics TableĀ 2.Outcomes of Endoscopic Ultrasonography-Guided Gallbladder Drainage TableĀ 3.Outcomes of the Procedures
TableĀ 4.Previous Reports on Endoscopic Ultrasonography-Guided Gallbladder Drainage (studies with 10 cases)
REFERENCES1. Isayama H, Kawabe T, Nakai Y, et al. Cholecystitis after metallic stent placement in patients with malignant distal biliary obstruction. Clin Gastroenterol Hepatol 2006;4:1148ā1153.
2. Hasan MK, Itoi T, Varadarajulu S. Endoscopic management of acute cholecystitis. Gastrointest Endosc Clin N Am 2013;23:453ā459.
3. Tsuyuguchi T, Itoi T, Takada T, et al. TG13 indications and techniques for gallbladder drainage in acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci 2013;20:81ā88.
4. Ito K, Fujita N, Noda Y, et al. Percutaneous cholecystostomy versus gallbladder aspiration for acute cholecystitis: a prospective randomized controlled trial. AJR Am J Roentgenol 2004;183:193ā196.
5. Giovannini M, Moutardier V, Pesenti C, Bories E, Lelong B, Delpero JR. Endoscopic ultrasound-guided bilioduodenal anastomosis: a new technique for biliary drainage. Endoscopy 2001;33:898ā900.
6. Baron TH, Topazian MD. Endoscopic transduodenal drainage of the gallbladder: implications for endoluminal treatment of gallbladder disease. Gastrointest Endosc 2007;65:735ā737.
7. Itoi T, Itokawa F, Kurihara T. Endoscopic ultrasonography-guided gallbladder drainage: actual technical presentations and review of the literature (with videos). J Hepatobiliary Pancreat Sci 2011;18:282ā286.
8. Itoi T, Binmoeller KF, Shah J, et al. Clinical evaluation of a novel lumen-apposing metal stent for endosonography-guided pancreatic pseudocyst and gallbladder drainage (with videos). Gastrointest Endosc 2012;75:870ā876.
9. de la Serna-Higuera C, PĆ©rez-Miranda M, Gil-SimĆ³n P, et al. EUS-guided transenteric gallbladder drainage with a new fistula-forming, lumen-apposing metal stent. Gastrointest Endosc 2013;77:303ā308.
10. Widmer J, Alvarez P, Gaidhane M, et al. Endoscopic ultrasonography-guided cholecystogastrostomy in patients with unresectable pancreatic cancer using anti-migratory metal stents: a new approach. Dig Endosc 2014;26:599ā602.
11. Jang JW, Lee SS, Song TJ, et al. Endoscopic ultrasound-guided transmural and percutaneous transhepatic gallbladder drainage are comparable for acute cholecystitis. Gastroenterology 2012;142:805ā811.
12. Choi JH, Lee SS, Choi JH, et al. Long-term outcomes after endoscopic ultrasonography-guided gallbladder drainage for acute cholecystitis. Endoscopy 2014;46:656ā661.
13. Takagi W, Ogura T, Sano T, et al. EUS-guided cholecystoduodenostomy for acute cholecystitis with an anti-stent migration and anti-food impaction system; a pilot study. Therap Adv Gastroenterol 2016;9:19ā25.
14. Tyberg A, Saumoy M, Sequeiros EV, et al. EUS-guided versus percutaneous gallbladder drainage: isnāt it time to convert? J Clin Gastroenterol 2018;52:79ā84.
15. Kamata K, Takenaka M, Kitano M, et al. Endoscopic ultrasound-guided gallbladder drainage for acute cholecystitis: long-term outcomes after removal of a self-expandable metal stent. World J Gastroenterol 2017;23:661ā667.
16. Choi JH, Kim HW, Lee JC, et al. Percutaneous transhepatic versus EUS-guided gallbladder drainage for malignant cystic duct obstruction. Gastrointest Endosc 2017;85:357ā364.
17. Irani S, Baron TH, Grimm IS, Khashab MA. EUS-guided gallbladder drainage with a lumen-apposing metal stent (with video). Gastrointest Endosc 2015;82:1110ā1115.
18. Walter D, Teoh AY, Itoi T, et al. EUS-guided gall bladder drainage with a lumen-apposing metal stent: a prospective long-term evaluation. Gut 2016;65:6ā8.
19. Kahaleh M, Perez-Miranda M, Artifon EL, et al. International collaborative study on EUS-guided gallbladder drainage: are we ready for prime time? Dig Liver Dis 2016;48:1054ā1057.
20. Irani S, Ngamruengphong S, Teoh A, et al. Similar efficacies of endoscopic ultrasound gallbladder drainage with a lumen-apposing metal stent versus percutaneous transhepatic gallbladder drainage for acute cholecystitis. Clin Gastroenterol Hepatol 2017;15:738ā745.
21. Dollhopf M, Larghi A, Will U, et al. EUS-guided gallbladder drainage in patients with acute cholecystitis and high surgical risk using an electrocautery-enhanced lumen-apposing metal stent device. Gastrointest Endosc 2017;86:636ā643.
22. Teoh AYB, Serna C, Penas I, et al. Endoscopic ultrasound-guided gallbladder drainage reduces adverse events compared with percutaneous cholecystostomy in patients who are unfit for cholecystectomy. Endoscopy 2017;49:130ā138.
23. Manta R, Mutignani M, Galloro G, Conigliaro R, Zullo A. Endoscopic ultrasound-guided gallbladder drainage for acute cholecystitis with a lumen-apposing metal stent: a systematic review of case series. Eur J Gastroenterol Hepatol 2018;30:695ā698.
24. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373ā383.
25. Frenkel WJ, Jongerius EJ, Mandjes-van Uitert MJ, van Munster BC, de Rooij SE. Validation of the Charlson comorbidity index in acutely hospitalized elderly adults: a prospective cohort study. J Am Geriatr Soc 2014;62:342ā346.
26. Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 1982;5:649ā655.
27. PeƱas-Herrero I, de la Serna-Higuera C, Perez-Miranda M. Endoscopic ultrasound-guided gallbladder drainage for the management of acute cholecystitis (with video). J Hepatobiliary Pancreat Sci 2015;22:35ā43.
28. Anderloni A, Buda A, Vieceli F, Khashab MA, Hassan C, Repici A. Endoscopic ultrasound-guided transmural stenting for gallbladder drainage in high-risk patients with acute cholecystitis: a systematic review and pooled analysis. Surg Endosc 2016;30:5200ā5208.
29. Itoi T, Sofuni A, Itokawa F, et al. Endoscopic transpapillary gallbladder drainage in patients with acute cholecystitis in whom percutaneous transhepatic approach is contraindicated or anatomically impossible (with video). Gastrointest Endosc 2008;68:455ā460.
|
|
