INTRODUCTION
Colorectal cancer (CRC) is one of the global health problems and is the third leading cause of morbidity and second leading cause of mortality from cancer worldwide [1,2]. In the United States and European countries, the incidence is in the range of 20ŌĆō40 per 100,000 population. In Asian countries, it varies widely (4.4 in India; 44.5 in Korea per 100,000) [1]. In one study that conducted CRC screening in one of the regions of Kazakhstan [3], the high number of CRC cases detected indicated the need for more screening programs. An increase in the incidence rate of this pathology was observed since 2011, with the introduction of CRC screening; stage-related data indicate the predominance of stages I and II.
Attention needs to be given to the ŌĆ£morbidity and mortalityŌĆØ rates, which indicates the level of the development of oncological services in a particular country. In developed countries with a high level of medical care, the mortality rate varies from 24.0%, in Korea, to 37.3%, in Sweden, indicating low mortality, which is an indicator of developed oncological services [1,2]. In developing countries, this figure ranges from 57.1%, in Kazakhstan, to 75.4%, in India, which indicates a rather high mortality rate and a low level of development of oncological services [2,4].
Modern colonoscopy must be carried out to diagnose precancerous changes and early forms of cancer. The use of modern diagnosis techniques allows the detection of pathological formations of even the smallest size, such as chromoscopy and narrow-spectrum, magnifying, and autofluorescent endoscopy. The clinical application of these diagnostic methods and detailed visualization of minor pathological changes in the large intestine are possible with methodic studies. An essential condition for ensuring the effective use of endoscopic techniques and improving the quality of colonoscopy is the routine use of modern diagnostic algorithms, which can improve diagnostic results and popularity of endoscopic examination.
SCREENING PROGRAM OF COLORECTAL CANCER IN KAZAKHSTAN
According to regional endoscopic screening reports, a retrospective analysis was conducted of the overall incidence of CRC in the regions of Kazakhstan from 2004 to 2018 among people aged 50ŌĆō70 years. Colorectal screening was implemented in Kazakhstan since the second half of 2011. Screening for CRC in Kazakhstan occurs in two stages, the first stage is a hemoccult test, and if the results are positive, the next step is total colonoscopy. The early stage of detection is carried out by specialized medical care centers (city and district polyclinics). Patients aged 50ŌĆō70 years, of both sexes, are subject to screening. In the city and district clinics, there are screening rooms that keep records of indicators, and local nurses and doctors examine the patients. In each regional oncologic center, there is a screening room that monitors the screening process and keeps a general record of the identified cases of CRC.
Furthermore, the Kazakh Institute of Oncology and Radiology is developing an improved cancer screening program to identify, record, and analyze cases of cancer [5]. The annual coverage of the studies ranges from 982,919 (as recorded in 2011) to 1,155,174 (as recorded in 2012) of both men and women aged 50, 52, 54, 56, 58, 60, 62, 64, 66, 68, and 70 years. The planned optimal coverage is 70% of the population according to the register of the assigned population. In 2018, this coverage was 64.4%. The number of CRC cases detected increased from 199 (min) in 2011 to 514 (max) in 2014, and in the last year, 309 cases were detected. Further, the level of detectability increased from 0.02% to 0.05%, which indicates an increase in the effectiveness of testing. In the last four years, cases of early forms of cancer increased up to 88.3% in 2018 [5]. The Kazakh Institute of Radiology and Oncology published a statement of endoscopic screening for CRC. The annual report revealed that cancer was detected by regional oncologic dispensaries and the patients were then transferred to the Kazakh Institute of Radiology and Oncology. A summary of the annual report was published by the Agency of Statistics and the Ministry of Health of Kazakhstan. In all regions of Kazakhstan, screening rooms were set up for the survey. The surveyed population was stratified by age and the presence of occult blood in feces. For residents of Kazakhstan, screening for CRC and removal of polyps during screening colonoscopy is part of the medical care for citizens. Screening studies are conducted only in public clinics, not private. According to the order of the Minister of Health of the Republic of Kazakhstan, dated December 25, 2017, Ōä¢ 995, ŌĆ£On approval of the rules of preventive medical examinations of the target populationŌĆØ, endoscopists during screening colonoscopy are obliged to simultaneously remove all neoplasms of 0-Ip and 0-Is types according to the Paris classification, measuring up to 0.5 cm [6]. Currently, cold snare, polypectomy, and endoscopic mucosal resection are prevalent technologies. The endoscopic submucosal dissection technology is available in very few clinics throughout the country, as this technology is costly and the practitioners have insufficient level of skills for its implementation. After starting of the screening program, the endoscopic equipment used in the field was analyzed in 2014. Karl StorzŌĆÖs endoscopic processors were purchased with the support of the Storz Professional Image Enhancement System using state funding.
INCIDENCE OF COLORECTAL CANCER IN OECD COUNTRIES AND KAZAKHSTAN
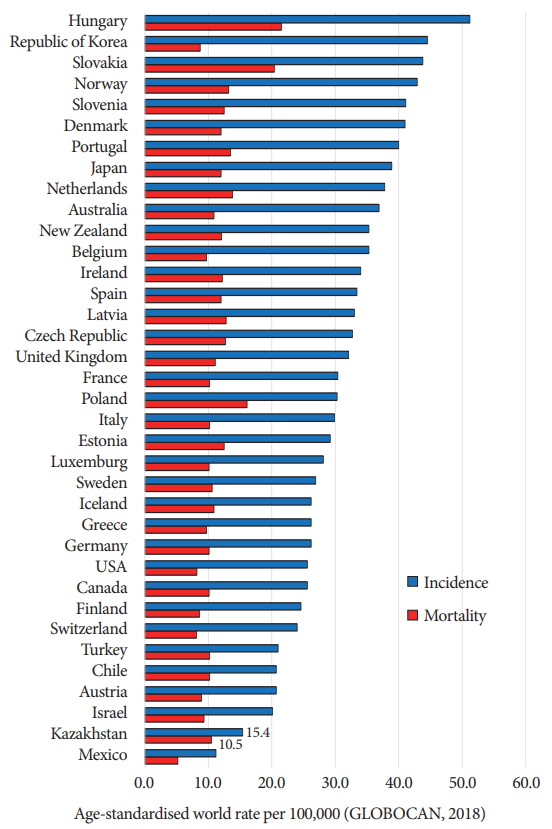
Fig. 1. shows that, according to Globocan (2018), the incidence of CRC in Organization for Economic Cooperation and Development (OECD) countries ranges from 11.2%, in Mexico, to 51.2%, in Hungary. Mortality from CRC in most OECD countries is in the range of 9%ŌĆō11%, except Hungary and Slovakia, where along with high morbidity, high mortality of up to 20%ŌĆō21.5% is reported. Low mortality rates were reported in Switzerland (8.1%), the United States (8.2%), the Republic of Korea (8.7%), and Mexico (5.2%). In terms of morbidity, Kazakhstan ranks almost last among OECD countries (15.4%). The ratio of mortality-to-morbidity of CRC in the Kazakhstan is 68.2%ŌĆöthe highest ratio for any OECD countryŌĆö followed by Poland (53.1%), with the lowest ratio reported in Korea (19.6%); further, the ratio is 32%ŌĆō33.8% in the US and Switzerland, 42% in Hungary, and 46.4% in Mexico. These statistics indicate the importance of CRC screening within Kazakhstan to detect early stages of cancer and reduce mortality.
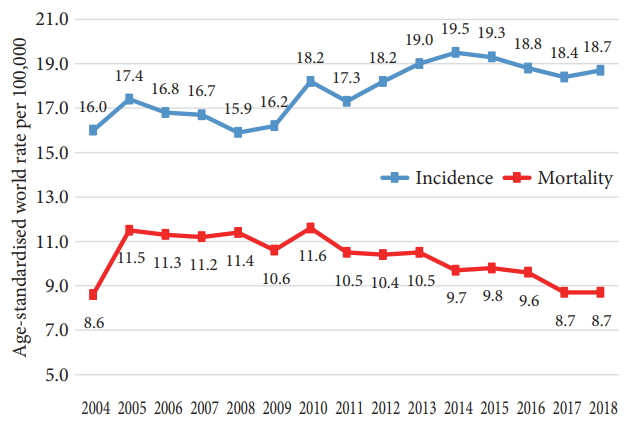
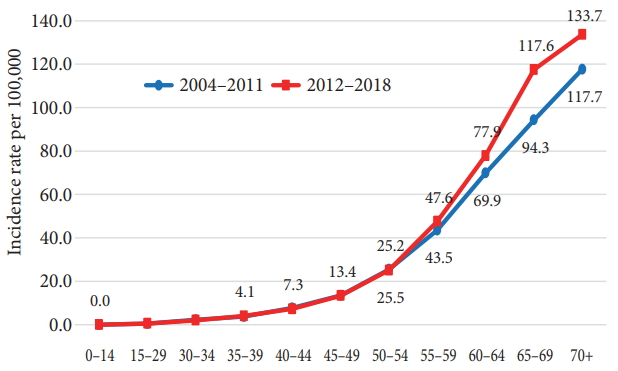
Fig. 2. shows the 15-year trend in morbidity and mortality from CRC. In the pre-screening period (2004ŌĆō2010), there were unstable indicators, with drastic growth and decline. Once the screening program was started, there was an increase in the cases of CRC (2011ŌĆō2014) with a further decrease and stabilization in the morbidity at 18.7% in 2018. The mortality curve in the pre-screening period was stable at the level of 11.2%ŌĆō11.5%. After the introduction of screening, there was a moderate but steady decline in mortality to 8.7 per 100 thousand population. The probability of CRC increased after the age of 40 years and sharply increased after 50 years in both screening (2004ŌĆō2008) and post-screening (2012ŌĆō2018) periods. The peak incidence in both periods was noted at the age of over 70 years; the incidence rate at the age of 65ŌĆō69 years increased from 94.3% to 117.6% and at the age of over 70 years from 117.7% to 133.7% (Fig. 3), respectively. With the introduction of screening, there has been a steady increase in the proportion of localized cancers (stage II) due to the reduction of locally advanced cases (stage III). Particularly noticeable growth in the early stages (from 49% to 57%ŌĆō60%) occurred since 2014 when the efficiency indicators of screening colonoscopy were introduced (Fig. 4).
TERRITORIAL FEATURES OF COLORECTAL CANCER IN KAZAKHSTAN
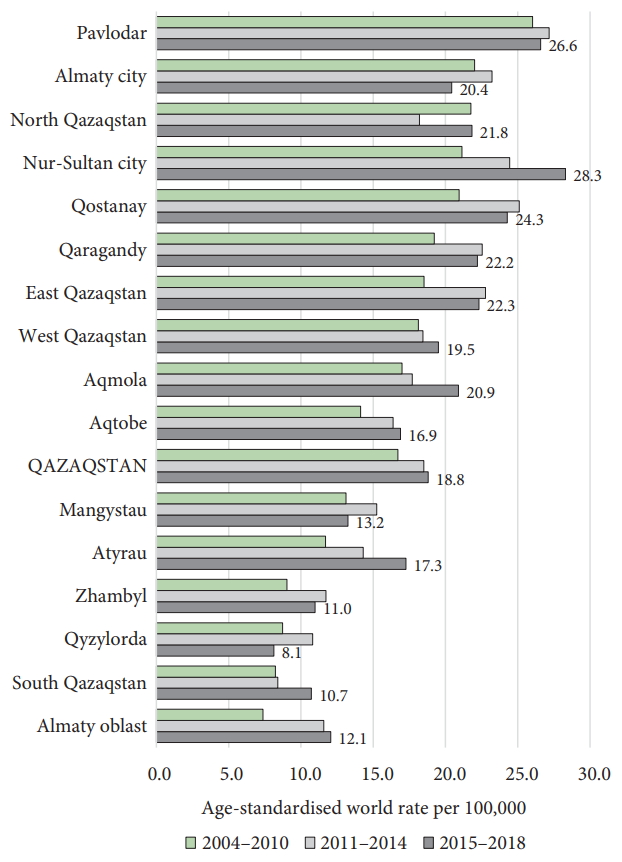
In Kazakhstan, the incidence of CRC shows territorial features. The territory of Kazakhstan is vast (Kazakhstan is the ninth largest country in the world), so there are geographical, economic, and cultural differences between the northern, western, and southern regions. According to the levels of morbidity (average annual rate for 2004ŌĆō2010), the regions of the country are divided into three groups: high (17%ŌĆō26%), mid (11.7%ŌĆō14.1%), and low (7.4%ŌĆō9.0%) rate. The northern, eastern, and central regions are classified under high rate. In these areas of Kazakhstan, red meat is consumed often, with similar food items/preparations, e.g., in Pavlodar, North Kazakhstan, Qostanay, Akmola region, Qaraghandy, East Kazakhstan, Nur-Sultan, West Kazakhstan, and Almaty (South region). Western Kazakhstan (Aktobe, Mangystau, Atyrau) showed an incidence in the mid-range; in this area, meat and fish are consumed often. Low rate was noted in the southern regions where vegetables and fruits are the traditional foods. The average annual morbidity in the region of Pavlodar (first rank) was 3.5 times higher than that in the region of Almaty (last rank among the territories). The figure shows the average annual levels of morbidity in the first (organizational) stage of the screening (2011ŌĆō2014) and in the stage of improving the quality of screening (2015ŌĆō2018) with the introduction of quality indicators of colonoscopy (Fig. 5). In the country, CRC incidence in the first stage of screening increased from 16.7% to 18.5% and then to 18.8%. The increase in morbidity was different in different regions. Effective screening was a factor resulting in an increase in the incidence of CRC. Table 1 compares the detection of cancer in the testing stages and the increase in the rate of CRC during the period of screening implementation in the regions of Kazakhstan. There was noted the influence of screening on the dynamics epidemiological indicators of CRC. One hundred twenty-three indicators of CRC were assessed using a six-point scale, where 0 denoted no influence of screening, 5 denoted strong impact (Table 1).
In Almaty and North Kazakhstan, high morbidity was reported with the introduction of CRC screening. Of note, in the group of high-morbidity regions, there were regions with stable and positive influence of screening (Nur-Sultan, East Kazakhstan, Qostanay, Qaragandy) as well as regions with low or insignificant influence. In contrast, of the four regions with low baseline morbidity, three showed a pronounced and robust impact of screening on the increase in morbidity; however, the detection rate was the same or lower than that in the country. On the other hand, the country-wide detection rate of CRC (0.04% of coverage) was high [5]. The surveyed population was the minimum in 2015, i.e., 791,904 people, and was the maximum in 2012, i.e., 1,174,155 people. Patients with positive hemoccult test results accounted for 1%ŌĆō4% of the total number of examined patients. The number of screening colonoscopies was the lowest in 2012 (33%) and the highest in 2014, equivalent to 81% of the total number of positive hemoccult test results (Table 1). There was a large number of patients with positive results on the hemoccult test during the introduction of the program, which can be explained by improper examination and the presence of false-positive results. There was also a discrepancy between the number of positive hemoccult test results and the number of screening colonoscopies, mainly because a large number of patients refused to undergo colonoscopy because it is performed without sedation. Unfortunately, the quality of screening is not equal to that in developed countries. The differences are due to the lack of advanced equipment, lack of trained personnel, and unavailability of resources for colonoscopy. Furthermore, the population is not informed about endoscopic procedures. In our opinion, the positive impact of screening depends on the quality of screening colonoscopy, the skills of the doctor, and quality of endoscopic equipment used. Unfortunately, some clinics still use fiber endoscopes although video endoscopes are being provided with the support of narrow band imaging (NBI). Further, not all doctors conduct total colonoscopy due to lack of training.
CONCLUSIONS
The result of the analysis shows an increase in the rate of CRC in Kazakhstan. The stage-by-stage distribution of morbidity indicates an increase in stages I and II since 2011. Since the introduction of screening, the incidence of CRC has grown. This growth indicates the positive result of CRC screening, which is associated with positive economic effects as the treatment of stages I and II is cheaper than that of stages III and IV. In addition, a decrease in the total number of primary CRC cases is the result of timely detection of precancerous bowel disease during screening colonoscopy and subsequent treatment. In our opinion, the launch of the national CRC screening program has had a positive effect not only on the health of the population but also on the quality of medical services, e.g., improved equipment, introduction of new methods of diagnosis and treatment, and increased professionalism of doctors. Last year, the national screening program was reviewed by World Health Organization experts, and they recommended further improvements. Currently, the plan is to supply endoscopic equipment, with the support of NBI Equipment, to all regional and state hospitals and oncology centers.