CME for
KSGE members
Han: Pancreatic Tail Mass: A Diagnostic Challenge
Quiz
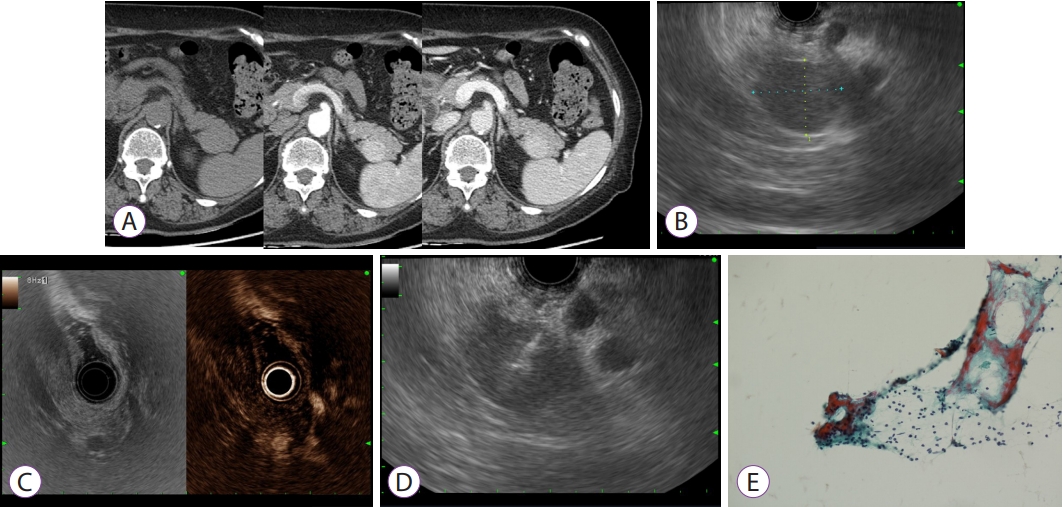
A 61-year-old female presented with an incidental finding of a pancreatic tail mass. She had been admitted for acute diarrhea and undergone abdominal computed tomography (CT) with contrast enhancement. CT showed a 2.6-cm, round, enhancing mass in the pancreatic tail ( Fig. 1A). The patient had been diagnosed with essential hypertension two years ago, and she was taking antihypertensive medication. She was a non-smoker and remained abstinent for 10 years. There was no unintentional weight loss, fever, or abdominal pain. Abdominal examination showed no palpable mass. Complete blood count and liver function tests were all within the normal range. The cancer antigen 19-9 level was 9.1 U/mL (reference: <37 U/mL). Endoscopic ultrasonography (EUS) with radial echoendoscope showed a 1.9 cm ├Ś 2.3 cm, round, hypoechoic mass with well-defined margins at the pancreatic tail ( Fig. 1B). There was no invasion of vascular structures or pancreatic duct dilatation. Contrast-enhanced EUS demonstrated homogenous enhancement of the mass ( Fig. 1C). EUS-guided fine needle aspiration (EUS-FNA) of the mass was performed ( Fig. 1D), but cytology did not reveal any malignant cells ( Fig. 1E). What is the most likely diagnosis?
Answer 
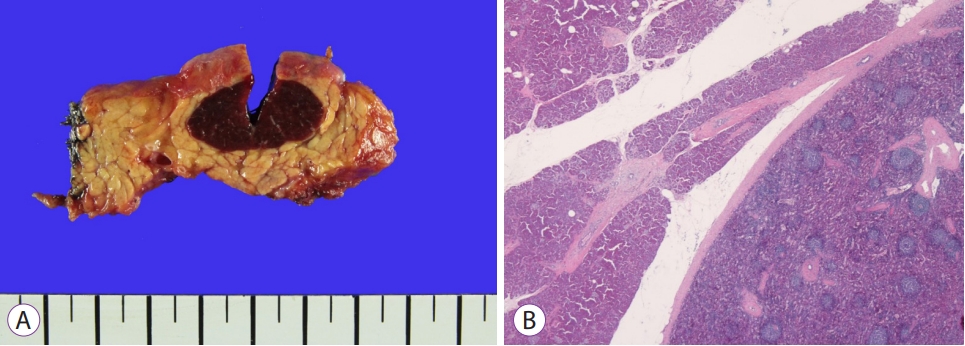
Given the presence of a round, enhancing mass in the pancreatic tail, pancreatic neuroendocrine tumor (NET) was strongly suspected. The patient underwent laparoscopic distal pancreatectomy. Gross appearance of the resected specimen showed a 2.3 cm ├Ś 1.5 cm, well-demarcated, dark brown mass in the pancreatic tail ( Fig. 2A). Microscopic findings revealed that the mass was surrounded by normal pancreatic tissue and composed of follicles and germinal centers ( Fig. 2B). The diagnosis was intrapancreatic accessory spleen.
Intrapancreatic accessory spleen
Accessory spleens can be found in about 10% of the population [ 1]. The most common location is the splenic hilum (80%), followed by the pancreatic tail (16.7%) [ 1]. There have been multiple reports of intrapancreatic accessory spleen mimicking pancreatic NET [ 1- 4]. Both accessory spleen and pancreatic NET show hyperattenuation in the arterial phase of contrast-enhanced CT. However, the attenuation of the accessory spleen remains stable throughout the arterial and portal venous phases, and the accessory spleen shows persistently high attenuation similar to that of the spleen. EUS-FNA can be helpful in obtaining tissue for pathological diagnosis, and 17.6% of intrapancreatic accessory spleen cases have been successfully diagnosed with EUS-FNA [ 1]. Chromogranin-A level is elevated in NETs, and its measurement can be helpful for differential diagnosis. However, elevated chromogranin-A level caused by chronic use of proton-pump inhibitors and liver cirrhosis was reported in a patient with intrapancreatic accessory spleen [ 4]. Somatostatin receptor scintigraphy and 68Ga-DOTA(0)-Phe(1)-Tyr(3)-octreotide positron-emission tomography/CT, which are used in the diagnosis and staging of NETs, can present false positive results in patients with intrapancreatic accessory spleen because of the presence of somatostatin receptors in the red pulp of the spleen [ 3, 4]. Notably, technetium-99m-labeled heat-damaged red blood cell scintigraphy is highly specific in detecting intrapancreatic accessory spleen [ 2, 3]. When a solid hypervascular pancreatic mass is incidentally found in the tail of the pancreas, intrapancreatic accessory spleen should be considered in the differential diagnosis. Detailed evaluation and accurate diagnosis could help avoiding surgery in this benign condition.
Fig.┬Ā1.
(A) Contrast-enhanced computed tomography demonstrates a 2.6-cm, round, enhancing mass in the pancreatic tail. (B) Endoscopic ultrasonography shows a 1.9 cm├Ś2.3 cm round hypoechoic mass with well-defined margin at pancreatic tail. (C) Contrast-enhanced endoscopic ultrasonography shows homogenous enhancement of the mass. (D) Endoscopic ultrasound-guided fine needle aspiration is performed. (E) Cytology shows no malignant cells. 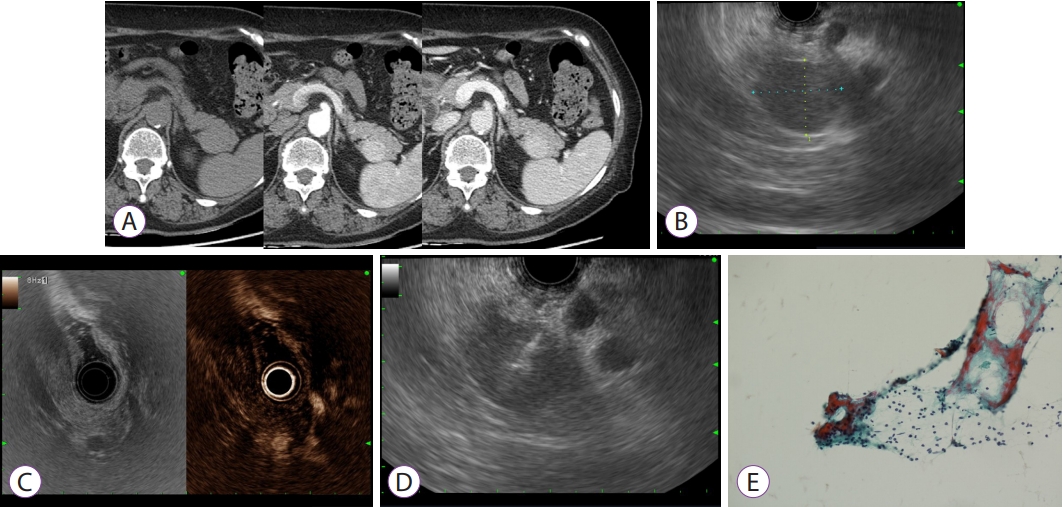
Fig.┬Ā2.
(A) Gross appearance of the resected specimen reveals a 2.3 cm├Ś1.5 cm well-demarcated, dark brown mass in the pancreatic tail. (B) Microscopic examination reveals that the mass is surrounded by normal pancreatic tissue and composed of follicles and germinal centers (hematoxylin and eosin stain, ├Ś20). 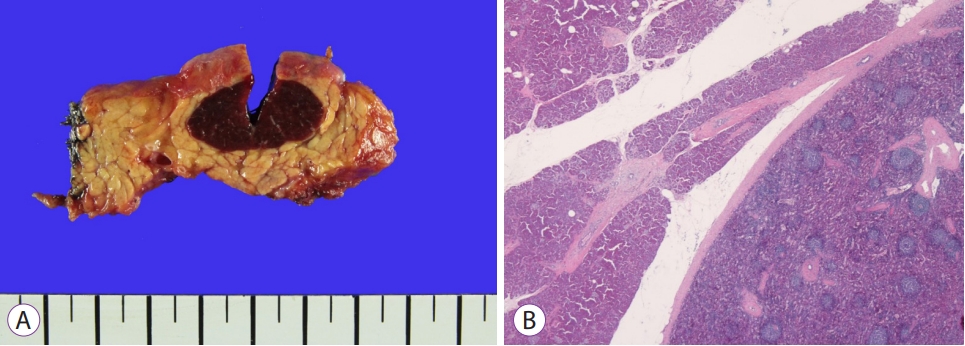
|
|