INTRODUCTION
Esophageal fibrovascular polyps (EFPs) are among the rarest benign esophageal tumors. In the available literature, only a few over 100 cases have been described.1 The predominant symptoms of polyps are dysphagia, regurgitation, vomiting, and nonspecific chest pain, which increase with polyp size. The tumor is typically located in the cervical part of the esophagus or hypopharynx, can reach a huge size, and in certain circumstances, can be life-threatening.2
Here, we present a method for endoscopic resection of giant EFPs. To our knowledge, this is the largest cohort of endoscopically treated patients in the literature.
CASE REPORT
Diagnostic
The diagnostic work-up included chest X-ray, barium swallow, chest computed tomography (Fig. 1), esophagoscopy with biopsy and endoscopic ultrasound.
Endoscopic technique
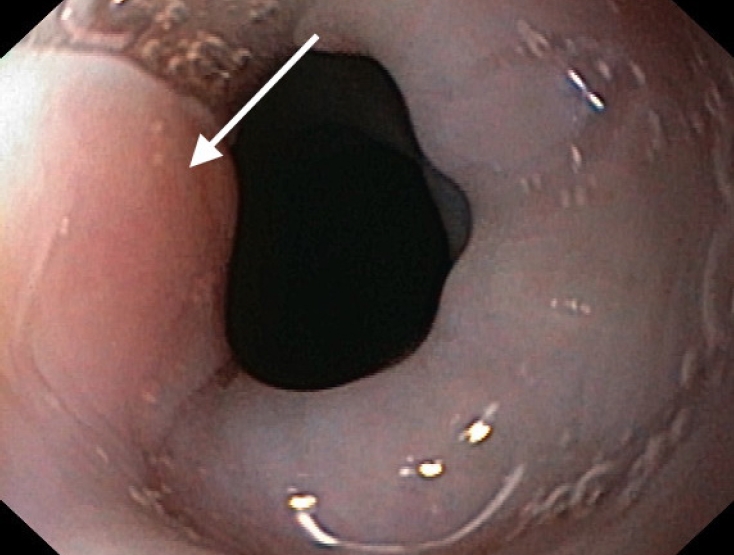
The procedure was performed under general anesthesia. First, the polyp base was evaluated during endoscopy, then a laryngoscope to visualize laryngopharynx with the stalk of the polyp, followed by moving the polyp outwards into the oral cavity and then outside using an endoscope and adjacent grasping tool (Figs. 2ŌĆō4). This maneuver enabled access to the base of the stalk for safe removal. Finally, the removal itself, under endoscopic control, was performed using diathermy, hot snare, and argon plasma coagulation. Endoscopic control was routinely performed on the first postoperative day. Patients were on a liquid diet, and the length of hospital stay varied between one and three days, although one patient stayed for 5 days for a thoracotomy.
Patient 1
A 54-year-old man presented with increased dysphagia, loss of appetite, vomiting, and unintentional weight loss of approximately 4 kg. Diagnostic work-up was performed as described above. Microscopy was suggestive of esophageal mucosal inflammation. He was admitted with acute dyspnea and dysphagia before the elective surgery. The patient was operated in an emergency setting. Endoscopy was performed under general anesthesia to localize the polyp origin. The polyp was removed as described above. On the first postoperative day, esophagoscopy was performed, which showed good healing at the post-polypectomy site. The patient was discharged on the third postoperative day. There were no signs of local recurrence during the follow-up period of 89 months.
Patient 2
A 48-year-old woman was admitted to the ward with complete dysphagia. After the diagnostic work-up, a giant esophageal polyp was diagnosed. Microscopy was suggestive of esophageal mucosal inflammation. Before surgery, an endocavitary electrode was implanted due to symptoms of bradycardia. Diagnostic endoscopy was performed under general analgesia, revealing a pedunculated polyp measuring 7├Ś3 cm. The patient was scheduled for endoscopic treatment, and the polyp was removed. On the first postoperative day, esophagoscopy was performed and showed good healing at the post-polypectomy site. There were no signs of local recurrence during the follow-up period of 81 months.
Patient 3
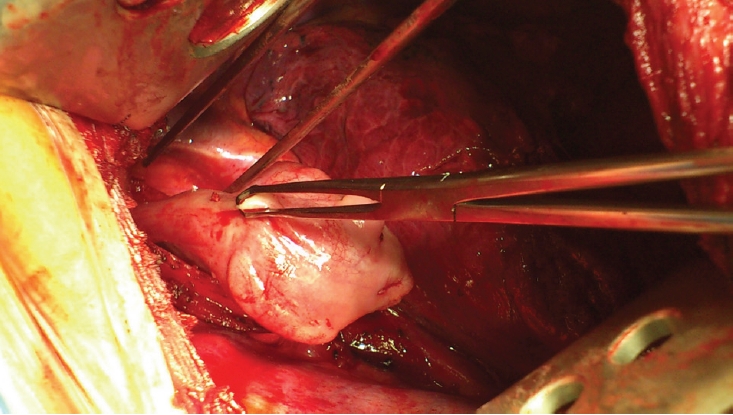
A 55-year-old man was admitted to Department of Thoracic and Surgical Oncolgy Jagiellonian University, John Paul II Hospital with dysphagia with the same diagnostic workup from previous patients. The results raised the suspicion of cancer; therefore, the patient was scheduled for surgery. Thoracotomy was performed. Intraoperatively, a giant esophageal polyp was diagnosed with no signs of malignancy in fresh frozen sections (Fig. 5). Removing the polyp was difficult during thoracotomy; therefore, the polyp measuring 9├Ś5 cm was removed endoscopically, as in the previously described cases. The patient was discharged home on the fifth postoperative day and was followed up for 77 months with no recurrence.
Patient 4
A 62-year-old woman was admitted to the hospital with acute symptoms of upper gastrointestinal tract bleeding. She received four units of packed red blood cells and achieved hemodynamic stability. A full diagnostic workup was performed after being transferred to our ward, as in the previous patients. The patient was scheduled to undergo endoscopic treatment, and then a 4├Ś3 cm polyp was removed. The patient was discharged home on the third postoperative day and was followed up for 48 months with no signs of local recurrence.
Patient 5
A 36-year-old man was referred to our department with an incidental finding of an esophageal lump, which was revealed on magnetic resonance imaging of the cervical spine performed for intervertebral disc disease. Esophagoscopy was performed with suspicion of an esophageal polyp. Repeated esophagoscopy revealed a 15 mm polyp with morphology suggestive of fibrovascular type; therefore, he was scheduled for a polypectomy. The postoperative period was uneventful, and the patient was discharged the following day. There were no signs of local recurrence during the follow-up period of nine months.
DISCUSSION
EFPs are among the least often diagnosed benign intraluminal esophageal lumps. They are often located on the posterior pharyngeal wall near LaimerŌĆÖs triangle or, more rarely, in the hypopharynx.3 Morphologically, the polyps are derived from the submucosal layer and are composed of muscular, vascular, fibrous, and adipose tissues.3 They may be asymptomatic or may cause different grades of dysphagia. Because of the stalk, they can regurgitate through the mouth and press on the larynx, which can lead to dyspnea and death.2 Esophageal polyps are usually correctly diagnosed during workup, but in approximately 25% of esophagoscopies, they are misdiagnosed due to their morphology.4 Furthermore, Graham et al.4 believe that correctly diagnosing esophageal polyps may not always be obvious, even after surgery, and that a differential diagnosis including liposarcoma should be considered.
Endoscopic techniques are the method of choice for patients with polyps at approximately 2 cm in diameter, while those >8 cm should be treated with open techniques.5 Giant polyps are those measuring >5 cm.5 Using a Vereda laryngoscope, Pham et al.6 resected a polyp measuring >10 cm. Ward et al.7 removed a 16├Ś3 cm polyp using an endoscopic loop technique. However, endoscopic removal of a polyp in its entirety is not always possible, and in some cases, it is difficult, as it may cause complications, which is confirmed by the reports of Li et al.8. The authors removed a 6 cm polyp in small parts without being sure of radicality, and the operation was interrupted due to edema of the esophageal mucosa after 3 hours. After a week, endoscopy was performed again, confirming radical removal.
Cockbain et al.9 presented the largest paper on open-technique treatment reported in the literature, involving four patients treated for EFPs. They believe that the open technique provides a good view of the pedicle, eliminates the risk of polyp recurrence, and should be reserved for patients with polyps measuring >10 cm. It should be noted that open-technique polyp removal was a major problem, and the authors used laparoscopy and gastrotomy to remove it. There was no recurrence during the long-term follow-up. Quijano et al.10 believe that the open technique is the method of choice for recurrent polyps.
It seems that one of the key elements in the treatment of patients with giant fibrovascular polyps is the identification of the polyp stalk and its correct resection. Improper stalk identification can lead to life-threatening complications, such as intraoperative bleeding or perforation of the esophageal wall or pharynx.
Our technique takes advantage of the mobility of the polyp, which is relocated to outside the mouth with a grasping instrument and is cut off under endoscopic guidance. Using this technique, we have a good view of the pedicle, allowing us to cut it off safely. No early perioperative complications, such as bleeding and/or esophageal fistula, or late complications related to polyp recurrence were observed after treatment.
EFPs are difficult to diagnose and treat. Our proposed method of transluminal polyp removal through the natural orifice is safe, allowing for the resection of large polyps. There were no signs of recurrence during the long-term follow-up. This technique could be the treatment of choice for EFPs, and only its failure should indicate open surgical treatment.