AbstractPortobiliary fistulas are rare but may lead to life-threatening complications. Biliary plastic stent-induced portobiliary fistulas during endoscopic retrograde cholangiopancreatography have been described. Herein, we present a case of portal cavernography and recurrent hemobilia after endoscopic retrograde cholangiopancreatography in which a portobiliary fistula was detected in a patient with portal biliopathy. This likely indicates a change in clinical presentation (from bilhemia to hemobilia) after biliary drainage that was successfully treated by placement of a fully covered, self-expandable metallic stent.
INTRODUCTIONInternal biliary fistulas are rare and occur in 0.9% to 3.2% of patients with hepatobiliary disease.1 This term generally refers to the communication of any part of the biliary tree with the gastrointestinal lumen, whereas fistula formation between the biliary tract and the portal vein is rare. The clinical manifestations of this type of fistula depend on both the etiology and type of fistula. Herein, we report a case of hemobilia due to a portobiliary fistula (PBF) in a patient with portal cavernoma. In addition, we report the results of a literature review that identified available evidence from previously reported cases.
CASE REPORTA 36-year-old male patient with polycythemia vera-induced portal vein thrombosis and cavernoma was referred to our hospital for endoscopic retrograde cholangiopancreatography (ERCP) due to recent onset of obstructive jaundice (bilirubin, 29 mg/dL). Cholestasis was mild (alkaline phosphatase, 160 U/L; gamma-glutamyl transferase, 52 U/L). He had no cholangitis (C-reactive protein, 4.2 mg/L), hemoglobin was 12.9 g/dL, and platelet count was 508,000/mm3. Abdominal magnetic resonance angiography demonstrated a portal cavernoma compressing the common bile duct (Fig. 1). ERCP with biliary sphincterotomy was performed, followed by 4-mm balloon dilation of a fibrotic stenosis associated with the biliary varices and placement of a straight plastic stent (10 cm, 10 French [Fr]). Two days later, the patient presented with melena, fever (38.4 °C), and a hemoglobin drop to 8.5 g/dL. Urgent endoscopy revealed fresh blood and clots in the duodenum. A second ERCP was performed and, after removing the stent, fresh blood from the papilla was observed (Fig. 2). After contrast injection, the portal venous system was opacified (portal cavernography) (Fig. 3A). Two straight plastic stents (9 cm, 8.5 Fr) were placed to bridge the stenosis and the PBF, while IV somatostatin was initiated. The patient remained stable and was discharged five days later, without further endoscopic control, on oral antibiotics and beta-blockers.
Two months later, the patient presented again with jaundice (bilirubin 9.9 mg/dL), melena (hemoglobin 9.6 g/dL), and chills. Abdominal computed tomography scan showed intrahepatic biliary duct dilation. During ERCP, after removal of the two occluded plastic stents, active bleeding was again observed and controlled after insertion of three biliary plastic stents (8.5 Fr). Unfortunately, 12 hours later, the patient developed hypovolemic shock, requiring intensive care unit admission. Another urgent ERCP determined again an opacification of the portal venous system (Fig. 3B) and a 60Ă10 mm fully covered, self-expandable metallic stent (FCSEMS) (Wallflex; Boston Scientific) was inserted (Fig. 4). The patient was discharged 2 weeks later with no bleeding recurrence or jaundice. Owing to the patientâs hemodynamic stability and favorable clinical condition, a second-look upper gastrointestinal endoscopy was not deemed necessary.
After the patient had been doing well for the next 6 months, the FCSEMS was replaced owing to occlusion with sludge, and no residual PBF was observed (Fig. 5A). Nine months later, the stent was removed without replacement, after balloon extraction of sludge and check for proper calibration of the stricture (Fig. 5B). Five months later, the patient was still in follow-up without relapse of bleeding, cholangitis, or jaundice.
DISCUSSIONPBF is a rare condition, and only a few case reports have been described in the literature. The first report of a PBF was in 1559,2 describing gallstones found in the portal vein of a patient who underwent autopsy. In our case, we believe that the fistula resulted from a bile duct wall injury that occurred during the index ERCP with balloon dilation. Other possible ERCP-related causes of trauma have also been reported, including biliary sphincterotomy, guidewire insertion, and stent placement (Table 1).3-14 Four of the 13 reported cases of ERCP-related PBF occurred in the setting of portal cavernoma.5,7,9
The major message to be taken from our experience is that in the case of PBF identified during ERCP, the optimal treatment should be the placement of a FCSEMS covering the PBF, at least if it is located in the middle or distal part of the common bile duct (to avoid the possibility of crossing the hilum with the risk of contralateral biliary obstruction). It is probable that the compression induced by FCSEMS favors thrombosis of biliary varices, a feature that cannot be achieved with plastic stents.
Other possible causes of PBF include blunt liver trauma, bile duct stone, liver abscess, malignancy, percutaneous transhepatic cholangiography, biliary surgery, transjugular intrahepatic portosystemic stent shunt, and percutaneous or transjugular liver biopsy.
PBF may result either in hemobilia, where blood enters the biliary tract, or more commonly, in the absence of portal hypertension and/or in case of untreated biliary stricture, in bilhemia, where bile enters the bloodstream. The pressure gradient between the biliary tree (10â15 mmHg) and the portal vein system (5â10 mmHg) explains the bilhemia. In our case, it is possible that bilhemia was already present before the index ERCP and that both the presence of portal hypertension and the treatment of biliary obstruction modified the clinical presentation towards hemobilia.
As previously illustrated, hemobilia associated with PBF may be a life-threatening condition. FCSEMS may be an acceptable and effective treatment option for both bleeding control and stricture calibration, as was seen in our case. Only three cases of PBF-induced hemobilia treated with FCSEMS have been described to date.7,9,14 In one of these cases, FCSEMS was complicated by recurrent cholangitis due to partial proximal stent migration.7 Other treatments that have been offered to control hemobilia in ERCP-related PBF include balloon tamponade, coil embolization, percutaneous or transjugular portosystemic stent placement, and surgical repair. However, transarterial embolization is not a good treatment option due to the venous origin of the bleeding.
In summary, this report describes a case of PBF that was identified during an ERCP performed for the treatment of a benign biliary stricture. Initial balloon dilation and plastic stenting treated the cholestasis (and possibly preexisting bilhemia) and induced recurrent and severe hemobilia, which was ultimately resolved by placement of a FCSEMS. This clinical presentation and possible treatment option should be kept in mind, especially for patients with portal hypertension presenting with elevated bilirubin levels and limited cholestasis.
NOTESFig. 1.(A) T2-weighted image (axial plane) depicting compression of the common bile duct between two venous structures (arrows). (B) T2-weighted image (coronal plane) showing a vessel as a low signal tubular structure (arrow) parallel to the common bile duct. 
Fig. 3.(A, B) Cholangiogram showing opacification of a venous structure compatible with the known cavernoma (black arrows) and contrast dye in a venous branch parallel to the bile duct (long white arrow) with possible orifice of portobiliary fistula (short white arrow). 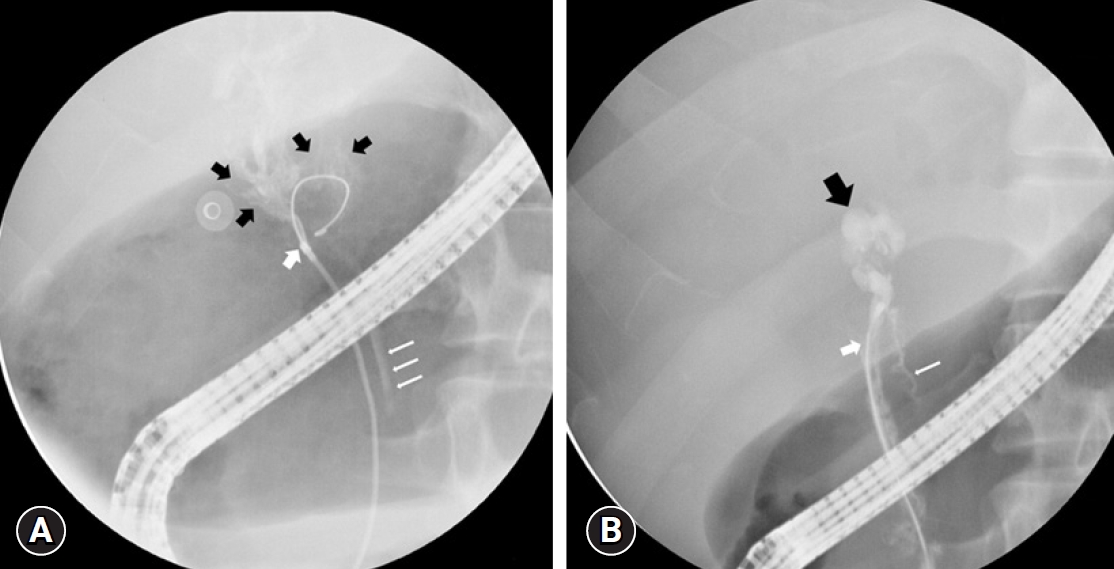
Fig. 4.Radiography showing the fully covered self-expandable metal stent deployed in the main bile duct. 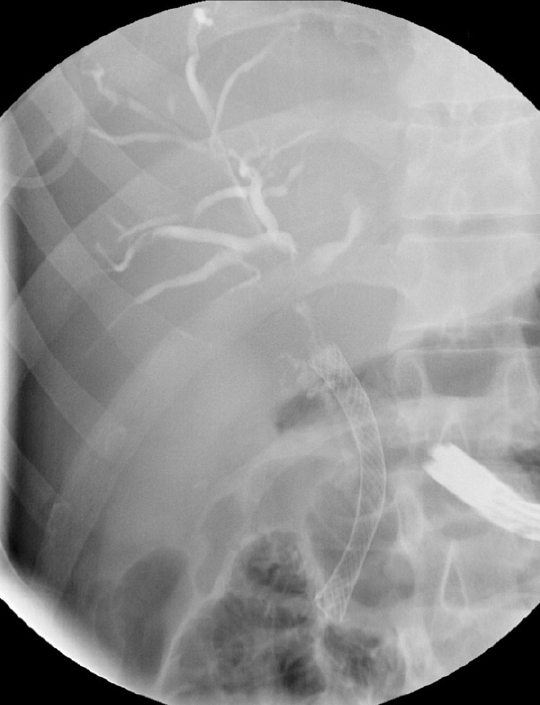
Fig. 5.(A) Radiography showing opacification of the common bile duct with no residual fistula during the endoscopic retrograde cholangiopancreatography performed to replace the initially placed fully covered self-expandable metal stent. (B) Radiography showing opacification of the common bile duct with no residual fistula or stenosis after definitive removal of the fully covered self-expandable metal stent. 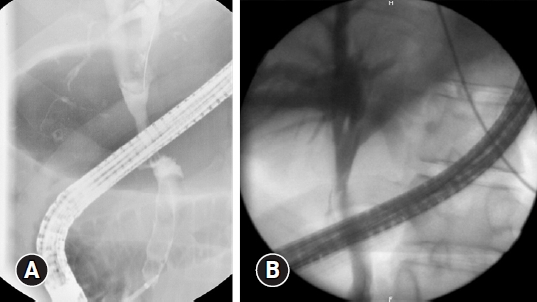
Table 1.Published case reports of ERCP-related portobiliary fistula
REFERENCES1. Yamashita H, Chijiiwa K, Ogawa Y, et al. The internal biliary fistula: reappraisal of incidence, type, diagnosis and management of 33 consecutive cases. HPB Surg 1997;10:143â147.
2. DiCocco JM, Fabian TC. Biliovenous fistula. In: Vincent JL, Hall JB, editors. Encyclopedia of intensive care medicine. Berlin: Springer; 2012. p. 303â305.
3. Huibregtse K, Gish R, Tytgat GN. A frightening event during endoscopic papillotomy. Gastrointest Endosc 1988;34:67â68.
4. Ricci E, Mortilla MG, Conigliaro R, et al. Portal vein filling: a rare complication associated with ERCP for endoscopic biliary stent placement. Gastrointest Endosc 1992;38:524â525.
5. Tighe M, Jacobson I. Bleeding from bile duct varices: an unexpected hazard during therapeutic ERCP. Gastrointest Endosc 1996;43:250â252.
6. Kennedy C, Larvin M, Linsell J. Fatal hepatic air embolism following ERCP. Gastrointest Endosc 1997;45:187â188.
7. Mutignani M, Shah SK, Bruni A, et al. Endoscopic treatment of extrahepatic bile duct strictures in patients with portal biliopathy carries a high risk of haemobilia: report of 3 cases. Dig Liver Dis 2002;34:587â591.
8. Espinel J, Pinedo ME, Calleja JL. Portal vein filling: an unusual complication of needle-knife sphincterotomy. Endoscopy 2007;39 Suppl 1:E245.
9. Layec S, DâHalluin PN, Pagenault M, et al. Massive hemobilia during extraction of a covered self-expandable metal stent in a patient with portal hypertensive biliopathy. Gastrointest Endosc 2009;70:555â556.
10. Furuzono M, Hirata N, Saitou J, et al. A rare complication during ERCP and sphincterotomy: placement of an endoscopic nasobiliary drainage tube in the portal vein. Gastrointest Endosc 2009;70:588â590.
11. Kawakami H, Kuwatani M, Kudo T, et al. Portobiliary fistula: unusual complication of wire-guided cannulation during endoscopic retrograde cholangiopancreatography. Endoscopy 2011;43 Suppl 2 UCTN:E98âE99.
12. Kalaitzakis E, Stern N, Sturgess R. Portal vein cannulation: an uncommon complication of endoscopic retrograde cholangiopancreatography. World J Gastroenterol 2011;17:5131â5132.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
