See commentary "Clinical and economic value of bispectral index monitoring for adequate endoscopic sedation" in Volume 55 on page 518 AbstractBackground/AimsBispectral index (BIS) monitors process and display electroencephalographic data are used to assess the depth of anesthesia. This study retrospectively evaluated the usefulness of BIS monitoring during endoscopic ultrasonography (EUS).
MethodsThis study included 725 consecutive patients who underwent EUS under sedation with propofol. BIS monitoring was used in 364 patients and was not used in 361. The following parameters were evaluated: (1) median dose of propofol; (2) respiratory and circulatory depression; (3) occurrence of body movements; (4) awakening score >8 at the time; and (5) awakening score 2 hours after leaving the endoscopy room.
ResultsThe BIS group received a significantly lower median dose of propofol than the non-BIS group (159.2 mg vs. 167.5 mg; p=0.015) in all age groups. For patients aged Ōēź75 years, the reduction in heart rate was significantly lower in the BIS group than in the non-BIS group (1.2% vs. 9.1%; p=0.023). Moreover, the occurrence of body movements was markedly lower in the BIS group than in the non-BIS group (8.5% vs. 39.4%; p<0.001).
INTRODUCTIONEndoscopic ultrasonography (EUS) is used to evaluate pathology inside and outside the gastrointestinal tract.1,2 Because the endoscope used for EUS is larger and the examination time is longer than that with conventional upper endoscopy, EUS requires sedation.3-7 A safe sedation method that minimizes body movements and respiratory and circulatory depression is desirable. To determine the appropriate dosage of sedatives during EUS, objective evaluation criteria must be established. Bispectral index (BIS) monitors process and display electroencephalographic data are used to assess the effects of general anesthesia during surgery.8,9 However, the utility of BIS monitoring for sedation management during short procedures, such as EUS, remains unclear. In this study, the value of BIS monitoring during EUS was retrospectively evaluated by assessing the effects of anesthesia in patients with or without BIS monitoring.
METHODSStudy designThis was a single-center, retrospective, comparative study. The primary endpoint was the safety and efficacy of BIS monitoring during EUS examination (Fig. 1). All methods were performed in accordance with the relevant guidelines and regulations.
PatientsThis study enrolled 725 consecutive patients (375 male and 350 female patients; median age, 64.9 years) who underwent EUS examination of extra- and intra-gastrointestinal tract pathology between January 2013 and September 2013. A BIS monitor was not used for approximately the first month of the study period, after which the use of the BIS monitor was assigned to patients on a random basis. BIS monitoring was used in 364 patients and not used in 361 patients (BIS group: between January 31 and September 16, 2013; non-BIS group: between January 4 and September 16, 2013). Patients were excluded if they met any of the following criteria: age<20 years, American Society of Anesthesiologists physical status score >5, allergy to midazolam or propofol, cranial nerve diseases, pregnancy, hypoxia with <90% arterial oxygen saturation on pulse oximetry (SpO2), systolic blood pressure (SBP) <90 mmHg, or heart rate (HR) <50 beats per minute (bpm).
Maintaining anesthesia with propofol during EUSThree physicians were involved in each EUS examination, each assigned a different role: one performed the EUS, one operated the ultrasound equipment, and one monitored the BIS signal and administered propofol. The physicians who administered propofol during EUS were first instructed by anesthesiologists. The EUS procedures were performed by experienced endosonographers, who had each performed more than 1,000 EUS procedures using an echoendoscope (GF-UCT260; Olympus Medical Systems, Tokyo, Japan). Patients received 2 L/min of oxygen during the procedure. Midazolam (0.04ŌĆō0.05 mg/kg) and propofol (2.0ŌĆō2.5 mg/kg) were administered to initiate sedation. Additional doses of propofol were administered in 20 mg increments until adequate induction of anesthesia was achieved. After initiating anesthesia, the endosonographers waited for a few minutes to confirm its effect, at which time EUS was started. To maintain sedation, propofol was intermittently administered at a dose of 20 mg based on body movements during EUS in the non-BIS group and on body movements and BIS values in the BIS group. The BIS values were maintained in the range of 60ŌĆō80. Patients who exhibited a rapid increase in the BIS value or a value >80 were administered an additional 20 mg dose of propofol by a physician other than the endoscopist. A biological information monitor was attached to all patients, and the pulse rate and SpO2 were continuously monitored during the examination. Blood pressure was measured at 5-minute intervals.
DefinitionsThe following parameters were compared between the two groups: (1) median dose of propofol; (2) respiratory and circulatory depression; (3) occurrence of body movements requiring discontinuation of the examination; (4) awakening score >8 at the time of leaving the endoscopy room; and (5) awakening score >8 at 2 hours after leaving the endoscopy room. Respiratory depression was defined as an SpO2 <90%. Circulatory depression was defined as an SBP of <90 mmHg and/or an HR <50 bpm. The awakening score was calculated according to the anesthesia recovery score, as shown in Table 1.10-12 The anesthesia recovery score was calculated using the following parameters: (1) motor activity, (2) respiration, (3) SBP, (4) level of consciousness, and (5) SpO2 saturation. Rest cancellation was possible at a recovery score of >8.
Statistical analysisContinuous variables were expressed as means┬▒standard deviation or as medians and ranges, and categorical variables were expressed as proportions. Continuous and categorical variables were analyzed using t-tests and chi-squared tests, respectively. Statistical significance was set at p<0.05. All statistical analyses were performed using SAS ver. 9.4 (SAS Institute, Cary, NC, USA).
RESULTSThe patient characteristics are shown in Table 2. There were no significant differences between the two groups in the male-to-female ratio or median examination time, but there was a significant difference in the average age. Table 3 presents the main results of the study. Overall (n=725), the BIS group received a significantly lower median dose of propofol than the non-BIS group (159.2 mg vs. 167.5 mg; p=0.015). The SpO2 drop was significantly lower in the BIS group than in the non-BIS group (13.7% vs. 20.2%; p=0.023). For patients aged <75 years (n=544), significant differences were found between the two groups in the reduction in SBP (11.3% in the BIS group vs. 17.6% in the non-BIS group; p=0.049), occurrence of body movements (46.8% vs. 43.5%; p=0.036), median dose of propofol (163.2% vs. 172.3%; p=0.027), and reduction in SpO2 (9.9% vs. 18.3%; p=0.006). These significant differences in respiratory and circulatory depression may be due to the age differences between the BIS and non-BIS groups. Patients aged Ōēź75 years (n=181) in the BIS group were older than those in the non-BIS group (Table 2). There was no significant difference in the propofol doses. Nevertheless, the decrease in HR was significantly lower in the BIS group than in the non-BIS group (1.2% vs. 9.1%; p=0.023). Moreover, the occurrence of body movements was markedly lower in the BIS group than in the non-BIS group (8.5% vs. 39.4%; p<0.001). There were no significant differences between the two groups in the awakening score at the time of leaving the endoscopy room or 2 hours thereafter in both the overall and subgroup analyses.
DISCUSSIONThe BIS monitor was the first electroencephalographic monitor to be approved for clinical use. It monitors brain waves using an electrode attached to the forehead, and the BIS value is calculated by analyzing the electroencephalogram. The BIS value is an estimate of the depth of anesthesia based on various brain wave components (relative ╬▓ ratio, SynchFastSlow, QUAZI, and burst suppression ratio).8 However, the reference database of brain waves was established using patients anesthetized using isoflurane, thiopental, propofol, or midazolam, combined with nitrous oxide or narcotics.9 Therefore, it is important to confirm the accuracy of BIS values in the presence of other anesthetic agents because BIS value association with the depth of sedation depends on the type of anesthesia used.9
The BIS value is calculated from signals acquired over the previous 60 seconds. Therefore, there is a delay between the value shown on the monitor and the actual value at that moment; hence, it is difficult to base an assessment of the depth of sedation exclusively on the BIS score. Nevertheless, the use of a BIS monitor can help to achieve the optimal depth of sedation by evaluating changes in the BIS value in individual cases. Use of the BIS monitor has been shown to reduce the dose/overdose of anesthetic agents and prevent side effects during surgical anethesia,13-16 lower digestive tract endoscopy, and endoscopic retrograde cholangiopancreatography.7-20
In this study, there was a significant reduction in respiratory depression in the non-BIS group, which may be related to the fact that the BIS group was younger than the non-BIS group. It is worth noting that BIS monitoring significantly reduced the amount of propofol used during the examination, even for younger individuals, and reducing the risk of overdose. There was no significant difference in the incidence of bradycardia or body movements, although BIS monitoring was associated with a decrease in these parameters. However, in patients 75 years of age or older, the occurrence of body movements was markedly lower in the BIS group than in the non-BIS group (8.5% vs. 39.4%; p<0.001). Moreover, the decrease in HR was significantly lower in the BIS group than in the non-BIS group (1.2% vs. 9.1%; p=0.023), although the patients in the BIS group were older. These results suggest that the BIS monitor can be used as an indicator of the depth of sedation, and thus help guide sedative dosage during endoscopic examination. Propofol is effective over a narrow range of concentrations in the blood and is difficult to maintain at an appropriate level. Thus, BIS monitoring may be particularly useful during EUS examination under propofol sedation. However, the degree of stimulus during EUS depends on the skill of the examiner, and it must be recognized that sedation using the BIS monitor requires a certain level of proficiency.
This study had several limitations. First, this was a retrospective study. There was no record of changes in BIS values during EUS; therefore, we could not determine how many patients exhibited rapid increases in BIS values or had values >80. It was not possible to control the physique, and/or situation during EUS in detail, although there may be various sources of bias in assessing these background factors. In addition, the degree of stimulus and pain experienced by patients differ according to the type of EUS examination. Finally, the difference in age between the BIS and non-BIS groups is a significant limitation. The present results and cost-effectiveness of BIS monitoring need to be confirmed under controlled conditions in future studies.
In conclusion, BIS monitoring is useful for maintaining a constant depth of anesthesia while reducing the dose of propofol. Especially for patients 75 years of age or older, the use of the BIS monitor might limit body movements and the reduction in HR that can occur during EUS examinations. The BIS monitor calculates the depth of anesthesia over a period of 60 seconds; therefore, sudden changes are not recorded in real time. The optimal depth of sedation can be determined by analyzing changes in the BIS value. However, respiratory and circulatory depression was observed even when the BIS monitor was used, and these effects should be addressed in future studies.
NOTESFig.┬Ā1.The bispectral index monitor analyzes the brain waves and displays the calculated bispectral index value at the bottom of the screen. 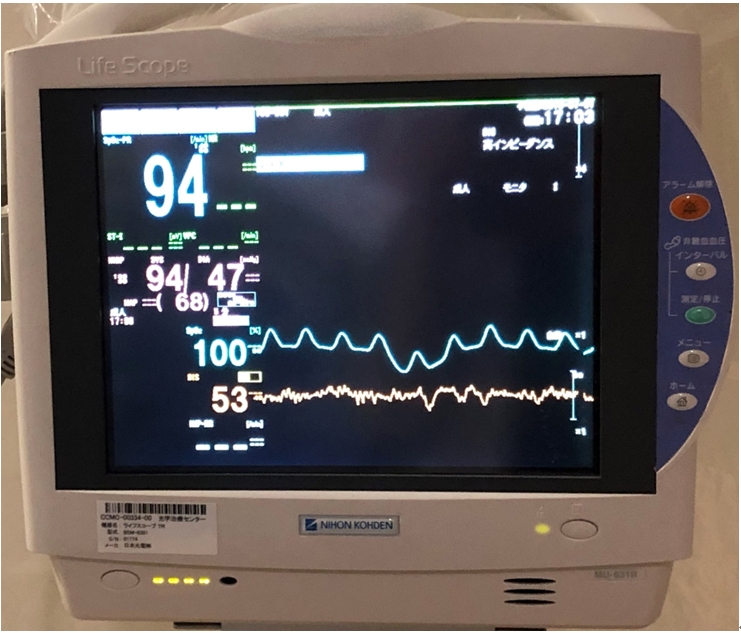
Table┬Ā1.Table┬Ā2.Patient characteristics Table┬Ā3.Principal results of this study
REFERENCES1. Kamata K, Takenaka M, Kitano M, et al. Contrast-enhanced harmonic endoscopic ultrasonography for differential diagnosis of localized gallbladder lesions. Dig Endosc 2018;30:98ŌĆō106.
2. Kamata K, Takenaka M, Kitano M, et al. Contrast-enhanced harmonic endoscopic ultrasonography for differential diagnosis of submucosal tumors of the upper gastrointestinal tract. J Gastroenterol Hepatol 2017;32:1686ŌĆō1692.
3. Cheriyan DG, Byrne MF. Propofol use in endoscopic retrograde cholangiopancreatography and endoscopic ultrasound. World J Gastroenterol 2014;20:5171ŌĆō5176.
4. Amornyotin S, Leelakusolvong S, Chalayonnawin W, et al. Age-dependent safety analysis of propofol-based deep sedation for ERCP and EUS procedures at an endoscopy training center in a developing country. Clin Exp Gastroenterol 2012;5:123ŌĆō128.
5. Lee TH, Lee CK, Park SH, et al. Balanced propofol sedation versus propofol monosedation in therapeutic pancreaticobiliary endoscopic procedures. Dig Dis Sci 2012;57:2113ŌĆō2121.
6. Pagano N, Arosio M, Romeo F, et al. Balanced propofol sedation in patients undergoing EUS-FNA: a pilot study to assess feasibility and safety. Diagn Ther Endosc 2011;2011:542159.
7. Yusoff IF, Raymond G, Sahai AV. Endoscopist administered propofol for upper-GI EUS is safe and effective: a prospective study in 500 patients. Gastrointest Endosc 2004;60:356ŌĆō360.
9. Glass PS, Bloom M, Kearse L, et al. Bispectral analysis measures sedation and memory effects of propofol, midazolam, isoflurane, and alfentanil in healthy volunteers. Anesthesiology 1997;86:836ŌĆō847.
11. Lovett P, G├│mez V, Hodge DO, et al. Propofol versus midazolam/fentanyl sedation for colonoscopy in the elderly patient population. J Perianesth Nurs 2017;32:210ŌĆō214.
12. Schmitz A, Weiss M, Kellenberger C, et al. Sedation for magnetic resonance imaging using propofol with or without ketamine at induction in pediatrics: a prospective randomized double-blinded study. Paediatr Anaesth 2018;28:264ŌĆō274.
13. Avidan MS, Zhang L, Burnside BA, et al. Anesthesia awareness and the bispectral index. N Engl J Med 2008;358:1097ŌĆō1108.
14. OŌĆÖConnor MF, Daves SM, Tung A, et al. BIS monitoring to prevent awareness during general anesthesia. Anesthesiology 2001;94:520ŌĆō522.
15. Gan TJ, Glass PS, Windsor A, et al. Bispectral index monitoring allows faster emergence and improved recovery from propofol, alfentanil, and nitrous oxide anesthesia. BIS Utility Study Group. Anesthesiology 1997;87:808ŌĆō815.
16. Choi WJ, Kim YH. How do you use bispectral index effectively for preventing re-awareness during general anesthesia? Korean J Anesthesiol 2012;62:1ŌĆō2.
17. Sandler NA, Hodges J, Sabino M. Assessment of recovery in patients undergoing intravenous conscious sedation using bispectral analysis. J Oral Maxillofac Surg 2001;59:603ŌĆō611.
18. Jang SY, Park HG, Jung MK, et al. Bispectral index monitoring as an adjunct to nurse-administered combined sedation during endoscopic retrograde cholangiopancreatography. World J Gastroenterol 2012;18:6284ŌĆō6289.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
