Kim, Kwak, Yoon, Jung, Kim, Boo, Oh, Jeon, Nam, Park, Park, Chun, Baek, Choi, Park, Byeon, Kim, Cho, Lee, Lee, Korean Society of Gastrointestinal Endoscopy, Korean Society of Gastroenterology, and Korean Association for the Study of Intestinal Diseases: Korean guidelines for postpolypectomy colonoscopic surveillance: 2022 revised edition
Abstract
Colonoscopic polypectomy is effective in decreasing the incidence and mortality of colorectal cancer (CRC). Premalignant polyps discovered during colonoscopy are associated with the risk of metachronous advanced neoplasia. Postpolypectomy surveillance is the most important method for the management of advanced metachronous neoplasia. A more efficient and evidence-based guideline for postpolypectomy surveillance is required because of limited medical resources and concerns regarding colonoscopy complications. In these consensus guidelines, an analytic approach was used to address all reliable evidence to interpret the predictors of CRC or advanced neoplasia during surveillance colonoscopy. The key recommendations state that the high-risk findings for metachronous CRC following polypectomy are as follows: (1) adenoma Ōēź10 mm in size; (2) 3 to 5 (or more) adenomas; (3) tubulovillous or villous adenoma; (4) adenoma containing high-grade dysplasia; (5) traditional serrated adenoma; (6) sessile serrated lesion (SSL) containing any grade of dysplasia; (7) serrated polyp of at least 10 mm in size; and (8) 3 to 5 (or more) SSLs. More studies are needed to fully comprehend the patients most likely to benefit from surveillance colonoscopy and the ideal surveillance interval to prevent metachronous CRC.
Keywords: Colonoscopy; Colorectal cancer; Guidelines; Polypectomy; Surveillance
INTRODUCTION
Colonoscopy is currently a key diagnostic modality for colorectal cancer (CRC) screening and the establishment of a treatment strategy. CRC remains one of the leading causes of cancer-related deaths worldwide, despite a decreasing trend in its incidence and mortality owing to the development of screening methods and prevention programs. 1 Screening methods to prevent CRC have been presented in various national cohort studies. Among the various methods, colonoscopic polypectomy, which involves the removal of colorectal polyps by colonoscopy, is reportedly the most effective method for reducing CRC incidence and CRC-related mortality. 2,3 Patients with colorectal polyps are at a high risk of developing colorectal polyps and CRC in the future; thus, appropriate surveillance using colonoscopy after colorectal polyp resection is instrumental. 4,5 Additionally, the significance of colonoscopic surveillance lies not only in detecting metachronous polyps but also in the detection of colorectal lesions not detected by index colonoscopy. In Korea, fecal occult blood test has been adopted as an item of national cancer screening program for CRC. However, colonoscopy has already been considered for efficient test for CRC screening because of the characteristics of the healthcare environment in Korea, defined by its high accessibility and utility of health services, leading to a remarkable increase in the detection and resection of colorectal polyps. 6 Although there is no doubt regarding the importance of postpolypectomy colonoscopic surveillance, the method may have a marginal effect on prevention compared to a screening colonoscopy; the likelihood of complications from colonoscopy is also present. Therefore, guidelines for the optimal practice of postpolypectomy colonoscopic surveillance, which maximizes the benefits and minimizes the possible damage, are required. 2,7,8 To establish Korea-specific guidelines, the Korean Society of Gastroenterology, Korean Society of Gastrointestinal Endoscopy, Korean Association for the Study of Intestinal Diseases, and Korean Society of Abdominal Radiology jointly organized a multi-society Taskforce Committee to develop national guidelines for colorectal polyp treatment. The Korean Guidelines for Postpolypectomy Colonoscopic Surveillance were first published in 2012 and distributed to health professionals for use in clinical practice. 9 Since establishing the first Korean guidelines, many studies have reported postpolypectomy colonoscopic surveillance, necessitating a revision of the existing Korean guidelines to reflect and incorporate additional evidence and reports. The revised edition of the Korean Guidelines for Postpolypectomy Colonoscopic Surveillance was developed by adapting three international guidelines that have been recently revised and released. 10-12 In this way, we aimed to present revised evidence-based guidelines that can be used as a useful reference to determine the timing and interval of colonoscopic surveillance, based on the assumption that the patient underwent a high-quality index colonoscopy conducted by experts in treating colorectal polyps. For the major recommendations in the revised guidelines, CRC incidence and mortality are set as the primary endpoints. The risk of developing metachronous advanced neoplasia, which was set as a key endpoint in previous guidelines, is considered a secondary endpoint. The estimates of benefits and risks are comprehensively considered in the revised guidelines. However, the revised guidelines exclude recommendations for follow-up of hereditary CRC (for example, hereditary non-polyposis CRC and familial adenomatous polyposis), inflammatory bowel disease, and serrated polyposis syndrome. Additionally, these guidelines do not take precedence over clinical evaluations made by physicians, taking into consideration of various factors related to patients and the healthcare environment in real-world clinical practice. Nevertheless, these guidelines are expected to serve as useful and complementary references in the clinical setting.
PROCESS OF GUIDELINE DEVELOPMENT
The guidelines are applicable to all patients (both men and women, including those with comorbidities) who have undergone colonoscopy and had polyps removed. The Guidelines Development Committee and Taskforce Committee include gastroenterologists and methodological experts as members to develop a revised edition of existing guidelines ( Appendix 1). By selecting reference guidelines through a systematic literature review and meta-analysis using a systematic process, the final guidelines were adapted for the development of this guideline. The guidelines developed in this study will be revised within the next 5 years, although early revision may be necessary in case of significant changes in the evidence base for the condition.
Development procedure
The guidelines were developed based on the Guidance for the Development of Clinical Practice guidelines ver. 1.0, as published by the National Evidence-Based Healthcare Collaborating Agency ( Appendix 2). The Guidelines Development Committee held its first meeting on July 6, 2020, and discussed the direction of revision for the existing guidelines. The guideline development process consisted of three stages: planning, development, and finalization. The planning stage consisted of (1) selecting the key themes of the guidelines; (2) reviewing the existing guidelines; (3) establishing a development plan; and (4) selecting key questions. The development stage consisted of (5) searching for evidence, quality assessment, and synthesis; (6) writing recommendations and determining the strength of recommendation; and (7) drawing consensus. The finalization stage consisted of an external review and publication of the final guidelines.
1) Selection of key questions
The Task Force Committee, consisting of nine members, reviewed three guidelines developed in the United States (US Multi-Society Task Force [USMSTF]), Europe (European Society of Gastrointestinal Endoscopy [ESGE]), and the United Kingdom (UK) (British Society of Gastroenterology [BSG]). First, twelve related themes were selected. Detailed key questions were determined considering the patient population (P), intervention (I), comparator (C), and outcome (O). Thus, the key questions that represent the building blocks of the recommendations are presented as PICO questions ( Appendix 2).
2) Search and selection of guidelines
The search for related literature was conducted by two taskforce members, using keyword terms for the guidelines. The major sources used for literature search included the international search engines PubMed, Ovid- Embase, and Cochrane libraries. A total of 503 guidelines published after 2015 were retrieved, after excluding duplicates. After reviewing titles and abstracts, 55 articles were selected. By reviewing the original texts of the articles, three guidelines that satisfied the following three conditions were finally selected: (1) guidelines including PICO that matched the key questions; (2) evidence-based guidelines that included the report of a systematic literature search and showed a clear connection between the recommendations and the supporting evidence; and (3) guidelines published in English ( Appendices 3, 4).
3) Final selection process of the guideline
Through a systematic literature review and inclusion/exclusion criteria, a quality assessment was conducted for the three guidelines published by USMSTF, ESGE, and BSG. All of them were selected as guidelines for adaptation ( Appendices 5, 6). 10-12 Quality assessment of the guidelines was performed based on the Korean Appraisal of Guidelines for Research and Evaluation II (K-AGREE II). In addition to comprehensive evaluation, scope and purpose, rigor of development, stakeholder involvement, clarity of presentation, applicability, and editorial independence were considered the key assessment domains. 13 Quality assessment of the guidelines using the K-AGREE II was performed by three taskforce members per guideline, and items with a difference of more than a specified score among taskforce members were refined through re-review and consensus discussion. For the final selection of the guidelines, rigor of development was considered with particular attention.
4) Writing process of the guideline
The recommendations and related evidence of the three guidelines selected by the Task Force Committee were comprehensively reviewed to derive the primary recommendations for the key questions ( Appendix 7), and the acceptance and applicability of these recommendations were evaluated ( Appendices 8, 9). Subsequently, the opinions of all the members were collected, and the final recommendations were compiled. For the level of evidence for each key question, major foreign grading methodologies, such as the Scottish Intercollegiate Guidelines Network, Grading of Recommendations, Assessment, Development and Evaluation, and existing domestic clinical practice guidelines, were reviewed. 14-17 After discussing with the Guidelines Development Committee, the level of evidence was divided into four, as shown in Table 1. To consider the level of evidence, the study design and quality assessment results of the selected studies were evaluated, and the consistency of the outcomes and precision of the evidence (total number of subjects or confidence intervals [CIs] in the included articles) were considered to determine the level of evidence for each key question. The strength of the recommendations was divided into four levels: strong recommendation, conditional recommendation, not recommended, and inconclusive ( Table 2). For content that lacked evidence or required clinical interpretation, the task force members held a consensus to reach an agreed conclusion. The level of evidence was divided into five, and the strength of the recommendation was determined by considering the level of evidence, benefits (such as clinical effects, increased patient satisfaction, and quality of life), and harm (such as adverse events, increased use of unnecessary resources, and decreased patient satisfaction). For cases in which quantitative synthesis of evidence was judged to be possible, a meta-analysis was performed, and the effect of a specific intervention on the outcome was presented using relative risk (RR), each with a 95% CI. Rex ver. 3.5.0. 2 (RexSoft Inc., Seoul, Korea; http://rexsoft.org/) was used for meta-analysis, with the ŌĆ£metaŌĆØ R package: Here, the I2 value ranges between 0 and 100%. An I2 value <25% indicates large homogeneity, I2 of 25% to 50% indicates low heterogeneity, I2 of 50% to 70% indicates medium heterogeneity, and I2 Ōēź70% indicates high heterogeneity. The final strength of recommendation was determined by consensus of Ōēź80% of the members in principle, but was ultimately determined based on the consent of all members of the Taskforce Committee.
5) Consensus and adoption of recommendations
After drafting the statements, the drafts were sent to experts in the relevant field by e-mail for review in advance, and necessary modifications were made through teleconferencing. A modified Delphi technique was used for the revised statements to draw a consensus among multi-society and multi-institutional experts for final confirmation ( Appendix 2).
Terms and definitions
In this guideline, based on the Korean Guidelines for Postpolypectomy Colonoscopic Surveillance published in 2012, the most commonly used terms were defined as follows, after referring to domestic and foreign studies. 9
1) Postpolypectomy surveillance: Colonoscopic examination to detect synchronous and metachronous polyps for removal before turning malignant after polypectomy. This term excludes the use of colonoscopy or other examinations to monitor for recurrence after CRC treatment. 2) Advanced adenoma: Adenomas Ōēź10 mm in size with high-grade dysplasia/tubulovillous or villous adenoma. 3) Advanced neoplasia Advanced adenoma or CRC. 4) Serrated polyp: The umbrella term used to describe hyperplastic polyps, sessile serrated lesions (SSLs), and traditional serrated adenomas (TSA) based on pathological diagnostic criteria. 5) Index colonoscopy: Colonoscopy was performed most recently before the surveillance colonoscopy. Index colonoscopy refers to a high-quality examination performed with adequate bowel preparation by colonoscopists who have received supervised endoscopy training above a certain level. 6) Adequate bowel preparation: There is no consensus on the definition of adequate bowel preparation. The ESGE defines adequate bowel preparation as follows: Boston Bowel Preparation Scale Ōēź6, Ottawa Scale Ōēż7, or Aronchick Scale excellent, good, or fair.11,18 7) High-quality examination: High-quality examination was defined based on various domestic and international guidelines and studies. Colonoscopy should be performed by a colonoscopist with an adequate adenoma detection rate (>30% for men, >20% for women). Patients undergoing colonoscopy should also undergo adequate bowel preparations. Colonoscopy should be performed up to the cecum, and the appropriate location (the entire cecum, ileocecal valve, and appendiceal orifice) should be determined. The examination is completed after observing the colonic mucosa during sufficient withdrawal time.10,19,20 8) Index adenoma: An adenoma that serves as the most fundamental reference for colonoscopic surveillance. Among the adenomas found during index colonoscopy, the adenoma with the most advanced pathological findings is set as the index adenoma; however, if the pathological findings are the same, the index adenoma refers to the largest adenoma.
Limitations of the revised edition of the Korean guidelines for postpolypectomy colonoscopic surveillance
Most studies used as evidence in this guideline were performed in Western countries, and the number of studies on the Korean population was limited. Additionally, most foreign studies used evidence from observational studies rather than randomized controlled trials (RCTs), which limits the quality of evidence for this guideline. Therefore, the task force undertook a Delphi meeting with clinical experts in colorectal polyps treatment to reflect the clinical setting in Korea and to explore metrics for treating colorectal polyps in clinical practice.
External review
An external review was conducted with experts from the Korean Society of Coloproctology who did not directly participate in developing this guideline to objectively verify the prepared draft. The outcomes of the external review can be found in the Appendix 10. After the review, the final statements were prepared and compiled by the Task Force Committee, documented after the final review by the Guidelines Development Committee; the final version of the guidelines was confirmed through a final review by the committee.
Distribution and implementation of the guidelines
The present guidelines will be published on the websites of relevant societies for viewing. Additionally, this guideline summarizes the latest trends and global evidence on postpolypectomy colonoscopic surveillance through systematic literature review and can be published in journals of relevant societies. The guidelines can also be used on various social media channels. To promote the implementation of the guidelines, a presentation in conference sessions is being considered, and changes in treatment patterns after releasing the guidelines will be monitored. We aim to monitor specific changes in treatment volume through open data sources, such as the Healthcare Big Data Hub ( opendata.hira.or.kr) or the Korea National Cancer Incidence Database.
Conflicts of interest
All members who participated in developing the guidelines disclosed their real and explicit interests related to the development activities. None of the members, including the chairperson of the Guidelines Development Committee, had experience in the development or approval process of the guidelines under review before the development of the present guidelines, nor had any relationship with companies associated with medicines, commodities, and services related to the guidelines within the two years before developing the guidelines. Those who received research grants did not participate in the discussion or voting process when the medications of the relevant company were discussed. The authors received no financial support from institutions or organizations other than the Korean Society of Gastrointestinal Endoscopy, Korean Society of Gastroenterology, and Korean Association for the Study of Intestinal Diseases.
SUMMARY OF RECOMMENDATIONS
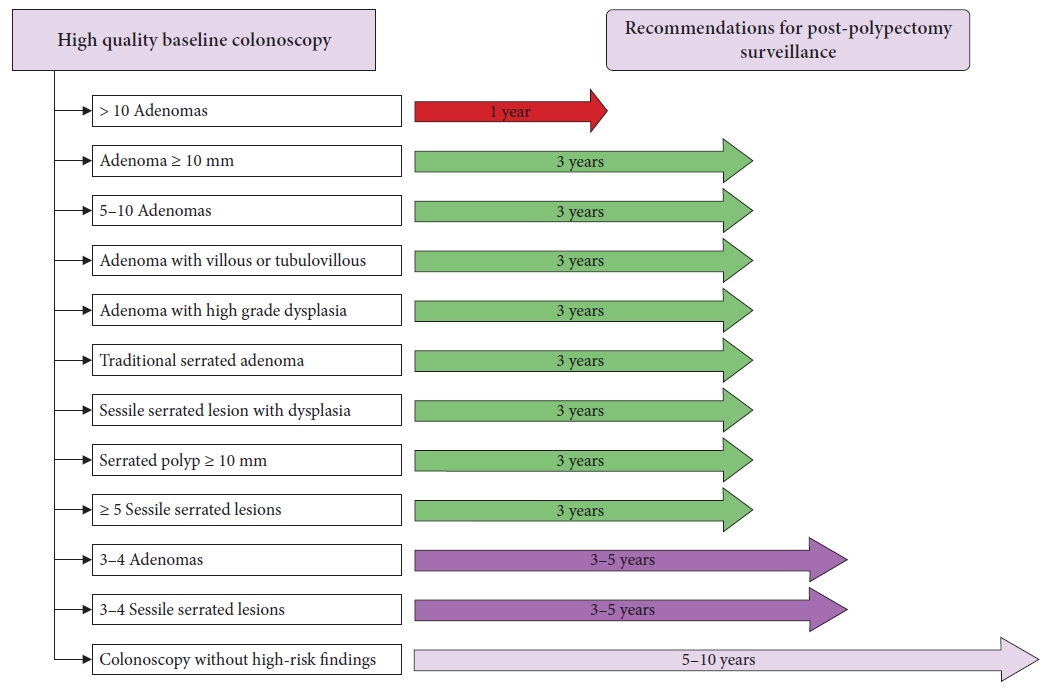
The guidelines assessed several risk factors to be reflected in determining the postpolypectomy surveillance interval and presented an appropriate surveillance interval based on the identified risk factors. The details of this summary are presented in Tables 3, 4.
KEY QUESTIONS AND RECOMMENDATIONS
What are the risk factors related to CRC incidence?
1) Is the size of tubular adenoma a risk factor to be considered when shortening the colonoscopic surveillance interval?
Statement 1. Shortening of the colonoscopic surveillance interval should be considered in patients with tubular adenomas Ōēź10 mm at index colonoscopy.
(Strength of Recommendation: Conditional recommendation; Level of Evidence: Low)
Similar to the 2012 domestic guidelines, a comprehensive review of studies reported since 2012 suggested that a large adenoma detected at index colonoscopy increased the future risk of advanced neoplasia development. 9 However, mixed results were reported depending on the cut-off size of the adenoma (10 mm vs. 20 mm). Overall, studies have shown consistency in that the index colonoscopy findings of adenomas >20 mm were associated with an increased risk of advanced neoplasia. However, with reference to adenoma size (10 mm), there were disparities in the reported results. In a retrospective multicenter cohort study conducted in the UK in 2017 that included 11,944 patients with intermediate-risk adenomas at index colonoscopy, surveillance colonoscopy was reported to reduce the risk of CRC incidence in the group with 1 to 2 adenomas Ōēź10 mm or 3 to 4 adenomas <10 mm. The protective effect of surveillance colonoscopy was pronounced in patients with incomplete colonoscopy, poor bowel preparation, adenomas with high-grade dysplasia or large adenomas (Ōēź20 mm), and proximal polyps at index colonoscopy. 21 However, in patients without these findings on index colonoscopy, the protective effect of surveillance colonoscopy was not significant. In a study that analyzed the Polish national CRC screening program, patients with adenomas Ōēź20 mm in size (standardized incidence ratio [SIR], 2.07; 95% CI, 1.40ŌĆō2.93) or with high-grade dysplasia (SIR, 0.79; 95% CI, 0.39ŌĆō1.41) showed a significant increase in the risk of CRC. 22 A study conducted in the UK in 2020 reported no significant increase in future CRC incidence for adenomas with a size of 10 to 19 mm compared with those <10 mm (hazard ratio [HR], 1.30; 95% CI, 0.75ŌĆō2.26). 23 However, in a recent cohort study, the risk of future CRC increased in both cases of tubular adenoma (HR, 2.54; 95% CI, 1.39ŌĆō4.64) and serrated polyps (HR, 2.82; 95% CI, 1.16ŌĆō6.82) when the size was Ōēź10 mm. 24 In a case-control study conducted in the US, adenomas Ōēź10 mm were significantly correlated with an increase in CRC incidence within 10 years of the examination (odds ratio [OR], 2.38; 95% CI, 1.53ŌĆō3.70). 25 In summary, the risk of future advanced neoplasia increases when a large adenoma is detected, and the risk increases with an increase in the size of adenoma at index colonoscopy. Most studies considered 10 mm as the reference value for adenoma size, which indicates an increased risk of future CRC; considering the recent reports that future advanced neoplasia increased in adenomas with a size of 6 to 9 mm compared with those with a size of 1 to 5 mm, 26,27 we used 10 mm as the cut-off value in this guideline, instead of 20 mm.
2) Is the number of colorectal adenomas a risk factor that should be considered when shortening the colonoscopic surveillance interval?
Statement 2. Patients with 3 to 5 non-advanced adenomas removed at index colonoscopy have the possibility of developing metachronous CRC and the risk of metachronous advanced neoplasia; therefore, shortening the surveillance interval should be considered.
(Strength of Recommendation: Conditional recommendation; Level of Evidence: Moderate)
Based on the results of recent large cohort studies, Western guidelines state that 3 to 4 non-advanced adenomas (NAAs) do not increase the risk of metachronous advanced neoplasia, similar to 1 to 2 NAAs detected at index colonoscopy. 11,12,21,22,28 Although the BSG guidelines define Ōēź5 NAAs as high-risk findings related to metachronous CRC, 12 the USMSTF guidelines still consider Ōēź3 NAAs as high-risk adenomas, citing insufficient research evidence on the risk of metachronous advanced neoplasia in patients with 3 to 4 NAAs. 10
Therefore, a meta-analysis was performed on previous cohort studies that evaluated the risk of metachronous advanced neoplasia and CRC between groups with the removal of 3 or Ōēź5 NAAs and those with the removal of 1 to 2 NAAs without other high-risk findings at index colonoscopy. Among the included studies, there were differences in terms of patient eligibility criteria, number of surveillance attempts, and duration of follow-up. It was also difficult to determine the status of colonoscopy quality, use of high-definition endoscopy, and timing of surveillance. These studies also had different primary endpoints, making consistent comparisons and analyses challenging. 21,26,29-38
Although there was statistical heterogeneity in the included studies, a meta-analysis of studies that included patients with 1 to 2 NAAs ( n=27,638), Ōēź3 NAAs ( n=4,973), and Ōēź5 NAAs ( n=991) at index colonoscopy showed that during a mean follow-up duration of 4.9 years, the advanced neoplasia incidence rates were 5.4%, 10.3%, and 10.0%, respectively ( Supplementary Fig. 1A). The RR of metachronous advanced neoplasia was 2.0 (95% CI, 1.78ŌĆō2.26; p<0.001; I 2=0%) and 2.2 (95% CI, 1.35ŌĆō3.73; p=0.002; I 2=62.2%), respectively, in the Ōēź3 NAAs or Ōēź5 NAAs group compared to the 1 to 2 NAAs group, indicating a significant increase in the risk of metachronous advanced neoplasia ( Supplementary Fig. 1B). Although there was a limitation in that only three retrospective cohort studies were included in the analysis, the RR of metachronous advanced neoplasia was 1.26 (95% CI, 1.05ŌĆō1.52; p=0.012; I 2=0%) in the 3 to 4 NAAs group compared to the 1ŌĆō2 NAAs group, indicating a statistical significance. In the Ōēź5 NAAs group compared to the 3 to 4 NAAs groups, the RR of metachronous advanced neoplasia was 1.96 (95% CI, 0.97ŌĆō3.96; p=0.060; I 2=68.0%), suggesting a statistical tendency ( Supplementary Table 1). When a meta-analysis was conducted with the incidence and RR of metachronous CRC, the incidence of CRC was 0.2%, 0.5%, and 0.1% in the 1 to 2 NAAs, Ōēź3 NAAs, and Ōēź5 NAAs groups, respectively ( Supplementary Fig. 2A). The RR of metachronous CRC was 1.80 (95% CI, 0.94ŌĆō3.45; p=0.077; I 2=0%) and 2.36 (95% CI: 0.22ŌĆō25.94, p= 0.481), respectively, in the Ōēź 3 NAAs and Ōēź 5 NAAs groups compared to the 1ŌĆō2 NAAs group. Thus, the RR of metachronous CRC increased with an increase in adenomas; however, this difference was not statistically significant ( Supplementary Fig. 2B). Additionally, the RR of metachronous CRC was 2.66 (95% CI, 0.39ŌĆō18.13; p=0.317; I 2=0%) in the 3 to 4 NAAs group compared to the 1 to 2 NAAs group, and the RR was 1.15 (95% CI, 0.14ŌĆō9.29; p=0.897; I 2=0%) in the Ōēź5 NAAs group compared to the 3 to 4 NAAs group, which was not statistically significant ( Supplementary Table 2). In summary, there was no statistically significant difference in the RR of metachronous CRC in the Ōēź3 or Ōēź5 NAAs group compared to that in the 1 to 2 NAAs group at index colonoscopy; however, the RR of metachronous advanced neoplasia showed a significant increase. Although there was no statistical difference in the RR of metachronous CRC in the Ōēź5 NAAs group compared to the 3 to 4 NAAs group, the RR of metachronous advanced neoplasia showed an increasing statistical tendency. If studies on high-quality colonoscopy with high-definition endoscopy can be conducted and accumulated over time, meta-analyses should be performed to re-evaluate the risk of metachronous advanced neoplasia and CRC in the 3 to 4 NAAs group.
Physicians must be careful for patients aged <60 years with Ōēź10 colorectal adenomas, Ōēź60 years with Ōēź20 adenomas, or Ōēź10 adenomas with a family history of CRC or polyposis, since these have a risk of CRC above the average risk for hereditary CRC syndrome or serrated polyposis syndrome. 12 The USMSTF, despite its weak strength of recommendation and incredibly low evidence, recommends surveillance colonoscopy after 1 year in patients with >10 adenomas removed at high-quality index colonoscopy. 10 In a single-center study conducted in Korea, which evaluated the metachronous advanced neoplasia in 214 patients with >10 adenomas removed compared with the group with 3 to 10 adenomas removed ( n=975), >10 adenomas were an independent risk factor for metachronous advanced neoplasia (OR, 2.25; 95% CI, 1.49ŌĆō3.38) during a 4.3-year follow-up. 39 Additionally, patients with >10 adenomas have an increased risk of developing familial adenomatous polyposis or MUTYH-associated polyposis. 40 Therefore, genetic testing is recommended considering various factors such as Ōēź10 adenomas or cumulative lifetime adenomas, age, family history of CRC, and comorbidities (for example, desmoid tumor, hepatoblastoma, a cribriform-morular variant of papillary thyroid cancer, and congenital hypertrophy of the retinal pigment epithelium). 41,42
3) Is a tubulovillous or villous adenoma a more influential risk factor that should be considered when shortening the colonoscopic surveillance interval compared to a tubular adenoma?
Statement 3. Shortening of the colonoscopic surveillance interval should be considered for patients who have tubulovillous or villous adenomas removed at index colonoscopy.
(Strength of Recommendation: Strong recommendation; Level of Evidence: Low)
For histological classification of the adenomas, adenomas with <25% of villous components are classified as tubular adenomas, those with Ōēź75% of villous components are classified as villous adenomas, and those between the two ranges are classified as tubulovillous adenomas. 43 According to the 2020 USMSTF guidelines, similar to the recommendation presented in 2012, removing adenomas with villous histology at index colonoscopy is a risk factor for developing advanced neoplasia in colonoscopic surveillance. 10 Fairley et al. 44 conducted a multicenter cohort study of 3,300 patients with adenomas removed during screening colonoscopy in Pennsylvania, USA. They found that patients with adenomas with villous histology had a higher risk of advanced adenoma and CRC incidence by 3.7-fold and 7.4-fold, respectively, compared to those without villous histology. In a multicenter study conducted in the Netherlands, a cohort of 2,990 patients diagnosed with adenoma during index colonoscopy was followed up for 4 years. The risk of advanced adenoma in colonoscopic surveillance doubled for patients with villous adenoma compared with those with one adenoma on index colonoscopy. 45 In the same study, the risk of advanced adenoma in colonoscopic surveillance was 2.1-fold and 1.7-fold in patients who had three adenomas and those with adenomas Ōēź10 mm, respectively, suggesting that villous adenoma at index colonoscopy is a risk factor for advanced adenoma in colonoscopic surveillance. According to a large-scale study in Sweden that evaluated the risk of CRC in patients with colorectal polyps ( n=178,377) compared to that in the general population ( n=864,831), the HR of CRC after 6.6 years of follow-up was 1.41 for patients with tubular adenoma, and 2.56 and 3.82 for those with tubulovillous adenoma and villous adenoma, respectively. 46 In a cohort study conducted in the US, 6,161 patients with adenomas were followed for approximately 10 years. Consequently, when patients with adenomas with villous histology at baseline index colonoscopy were compared to those without polyps, the HR of CRC incidence was 3.17 for tubulovillous adenoma and 8.51 for villous adenoma, showing a remarkably high HR. For those with 1 to 2 adenomas <10 mm in size, the HR of CRC incidence was high (2.91) for adenomas with villous histology; however, the risk of CRC incidence was not significantly high for tubular adenomas. 24 In the same study, the HR of CRC incidence were 3.15, 3.40, and 5.95 for 3 to 10 adenomas, adenomas Ōēź10 mm in size, and adenomas with high-grade dysplasia, respectively. It can be inferred that adenomas with villous histology at index colonoscopy are a clear risk factor for CRC incidence. Although the 2013 ESGE guidelines included an adenoma with villous histology at index colonoscopy as a high-risk group for CRC incidence and mortality at long-term follow-up, based on several recent studies reporting that the risk of CRC was not high, an adenoma with villous histology was excluded from the high-risk group in the revised 2020 guidelines. 11 According to a meta-analysis conducted by Saini et al., 47 when tubulovillous adenoma or villous adenoma was removed at baseline index colonoscopy, the RR of advanced adenoma in colonoscopic surveillance after 3 to 4 years of follow-up was not significantly higher compared to those patients who had tubular adenoma removed (RR, 1.26; 95% CI, 0.95ŌĆō1.66). According to a multicenter, retrospective cohort study conducted in the UK by Atkin et al., 21 the CRC incidence after the removal of villous adenoma at baseline index colonoscopy was not significantly higher than that after the removal of tubular adenoma during the 8-year follow-up period (HR, 1.16; 95% CI, 0.71ŌĆō1.91). Furthermore, the low level of interobserver consistency among pathologists in diagnosing villous histology in adenomas is also considered an important factor. 48
Similarly, in the UK, because of the low consistency among pathologists in its evaluation, villous histology has not been included in the BSG guidelines from a previous version, and it has been excluded from the definition of advanced adenoma. 12,49 However, the BSG guidelines stated that tubulovillous adenoma or villous adenoma detected on index colonoscopy is a risk factor for advanced adenoma and CRC in the first colonoscopic surveillance, and acknowledged consistency in the supporting evidence. It is generally known that the proportions of tubulovillous and villous adenomas among adenomas are 10% to 15% and 5% to 10%, respectively. 50 A study in the US by He et al. 24 reported the proportion of tubulovillous adenoma and villous adenoma to be 19% and 4%, respectively, while a study in the UK conducted by Atkin et al. 21 reported a proportion of 47% and 10%, respectively. The reason for the high proportion of adenomas with villous histology in the study by Atkin et al. was that patients with intermediate-risk adenomas were the participants in their study, and Ōēź90% of adenomas had a size Ōēź1 cm. When the ESGE and BSG guidelines excluded adenomas with a villous component from the high-risk group for CRC incidence during surveillance, the study by Atkin et al. 21 was presented as supporting evidence. However, as this study was conducted on patients with intermediate-risk adenomas, and consequently, there was no significant difference in the CRC incidence between the tubular adenoma and villous adenoma groups, careful interpretation of the results is required. In conclusion, each foreign guideline provides different perspectives on whether villous tissue is considered a high-risk finding associated with CRC following polypectomy. However, given that the USMSTF still considers villous tissue to be a risk factor and that relatively recent research findings corroborate this assertion, we opted to include tubulovillous/villous adenoma as a risk factor in this guideline.
4) Is a serrated polyp a risk factor that should be considered when shortening the colonoscopic surveillance interval?
Statement 4. Colonoscopic surveillance interval should be considered for shortening in a patient if a SSL with risk factors was removed during index colonoscopy.
(Recommendation: Inconclusive; Level of Evidence: Low)
To date, there have been no long-term prospective studies on mortality due to CRC and advanced neoplasia in patients with SSLs on index colonoscopy. Macaron et al. 51 reported no evidence supporting an increased risk of advanced neoplasia on surveillance colonoscopy after index colonoscopy with SSLs. However, a case-control study conducted by Erichsen et al. 52 suggested that in patients with an SSL and SSL with dysplasia on index colonoscopy, the risk of CRC increased by 3- and 5-fold, respectively, compared to that in patients with normal index colonoscopy. However, the study findings were limited by the fact that it was unknown whether SSLs were removed on index colonoscopy. In a cohort study by Holme et al., 53 the risk of CRC in patients with serrated polyps >10 mm on index sigmoidoscopy increased by 4.2-fold and 2.5-fold compared to that in patients with no adenoma on index sigmoidoscopy and no index sigmoidoscopy, respectively. However, this study had limitations because only 81 patients were included. Moreover, it is uncertain whether the results could be extended to SSLs during colonoscopy. Therefore, based on the available results, SSLs on index colonoscopy appear to increase the risk of CRC and advanced neoplasia. 24,54-59 However, the RR and risk factors for CRC and advanced neoplasia compared to tubular adenoma have not been conclusively documented. TSA, 60 SSLs larger than 10 mm, 58,61-67 and SSLs with dysplasia 57,68 have a higher risk for CRC and advanced neoplasia than SSLs without dysplasia and <10 mm. Recent guidelines by USMSTF and BSG recommended shortening the colonoscopic surveillance interval if Ōēź5 SSLs without dysplasia and <10 mm were removed compared to 1 to 4 SSLs without dysplasia and <10 mm. 10,12 Therefore, these factors can be defined as high-risk for CRC and advanced neoplasia if accompanied by a serrated polyp. Each factor is described as follows. According to previous observational studies, a hyperplastic polyp detected on index colonoscopy does not increase the risk of CRC or advanced neoplasia. However, these studies are limited because the analyses were not performed according to the size and location of hyperplastic polyps. 54,69 The risk of CRC and advanced neoplasia reportedly did not increase with small hyperplastic polyps in the sigmoid colon and rectum on index colonoscopy compared with normal index colonoscopy. 9,70 However, Schreiner et al. 58 reported that if a hyperplastic polyp or SSL was found in the right colon on index colonoscopy, the risk of synchronous advanced neoplasia increased by 1.9-fold, and the risk of adenoma on surveillance colonoscopy increased by 3.14-fold. Lim et al. 71 reported a 4.8-fold increased risk of advanced neoplasia with a hyperplastic polyp >6 mm in the left colon on index colonoscopy.
5) Is a TSA a risk factor that should be considered when shortening the colonoscopic surveillance interval?
Statement 5. Shortening of the colonoscopic surveillance interval should be considered for patients who had TSA removed at index colonoscopy.
(Strength of Recommendation: Conditional recommendation; Level of Evidence: Low)
TSAs are lesions with a risk of developing advanced neoplasia; however, there is a lack of supporting evidence. In a Danish cohort study comparing 2,045 patients with CRC and 8,105 controls, the number of patients with TSAs at baseline index colonoscopy was 14 (0.7%) and 17 (0.2%), respectively, and the adjusted OR was 4.84 (95% CI, 2.36ŌĆō9.93). 52 In a prospective cohort study of 12,955 patients aged 50 to 64 years who underwent colonoscopy screening, 81 had serrated polyps Ōēź10 mm in size. The group with large serrated polyps had a higher risk of CRC incidence than the group without polyps (HR, 4.2; 95% CI, 1.3ŌĆō13.3); thus, large serrated polyps were identified as an independent risk factor for CRC incidence (HR, 3.3; 95% CI, 1.3ŌĆō8.6). 53 However, among the 81 patients, only one was diagnosed with TSA. In a comparative cross-sectional study, the incidence of polyps was compared between 186 patients with TSA and 372 patients with adenoma. The incidence of high-risk adenomas was higher in the TSA group (adjusted OR, 2.37; 95% CI, 1.55ŌĆō3.63). 60 To summarize the studies on patients with TSAs discussed above, no previous study has compared only patients with TSAs with the normal group, and even studies that included patients with TSAs had fewer participants. Therefore, the BSG and ESGE guidelines consider TSAs as lesions with a high CRC or advanced neoplasia incidence, as in the case of adenomas such as serrated polyps Ōēź10 mm in size and serrated polyps with dysplasia. These guidelines recommend colonoscopic surveillance 3 years after index colonoscopy; however, the risk of TSA has not been mentioned separately. In the USMSTF guidelines, colonoscopy surveillance was recommended 3 years after removing TSAs; however, the strength of the recommendation and level of evidence was low. Considering the above recommendations in other guidelines, TSAs are presented as conditional recommendations in the current guideline.
6) Is histology of sessile serrated lesion with dysplasia a risk factor that should be considered when shortening the colonoscopic surveillance interval?
Statement 6. Shortening the colonoscopic surveillance interval should be considered for patients who had SSLs with dysplasia removed at index colonoscopy.
(Strength of Recommendation: Conditional recommendation; Level of Evidence: Very low)
In a nationwide population-based, nested case-control study in Denmark, the OR for future CRC incidence in SSL with dysplasia was approximately 5-fold compared to the cases without polyps (OR, 4.76; 95% CI, 2.59ŌĆō8.73); the estimated 10-year risk of CRC was 4.43% for patients with SSL with dysplasia, which was higher than the 0.93% in the group without polyps. However, in addition to being a case-control study, another limitation is that, since this study was conducted based on pathological findings only, it was not confirmed whether the polyps detected at baseline index colonoscopy were completely removed. 52
In another prospective cohort study, patients with SSLs with dysplasia at baseline index colonoscopy showed a 9-fold higher incidence of metachronous conventional adenomas compared to controls (RR, 9.03; 95% CI, 1.03ŌĆō16.03); however, there was no significant increase in the development of advanced adenoma (RR, 1.00; 95% CI, 0.15ŌĆō4.32). 72 Careful interpretation of the results is required because these are the secondary endpoints of the study, and the number of SSLs with dysplasia was small. In another retrospective cohort study, high-risk SSLs (SSLs Ōēź10 mm in size or SSLs with dysplasia) did not correlate with advanced neoplasia at follow-up colonoscopy (HR, 0.57; 95% CI, 0.14ŌĆō2.30). 55 However, this study has limitations in that the number of participants with high-risk SSL was only 27, and there were no data on the number of participants with SSLs with dysplasia. To summarize, there is insufficient evidence to determine whether SSLs with dysplasia increase the risk of advanced adenoma and CRC incidence at follow-up colonoscopy. However, SSLs with dysplasia have more histological features consistent with CRC than those without dysplasia. Therefore, we recommend that SSLs with dysplasia be considered high-risk until more evidence is gathered, and these patients undergo repeat colonoscopy within 3 years. Similarly, the USMSTF, ESGE, and BSG guidelines published in 2020 recommended a 3-year surveillance colonoscopy for patients with SSLs with dysplasia. 10-12
7) Is the size of a serrated polyp a risk factor that should be considered when shortening the colonoscopic surveillance interval?
Statement 7. Shortening the colonoscopic surveillance interval should be considered for patients who were found to have serrated polyps Ōēź10 mm at index colonoscopy.
(Strength of Recommendation: Conditional recommendation; Level of Evidence: Very low)
According to a population-based RCT ( n=100,210) in Norway from 1999 to 2011, when serrated polyps Ōēź10 mm in size were detected at index colonoscopy, the risk of CRC incidence increased by 4.2-fold compared to those without polyps (HR, 4.2; 95% CI, 1.3ŌĆō13.3). Moreover, a multivariate logistic regression analysis revealed that a serrated polyp Ōēź10 mm was an independent risk factor for future CRC incidence (OR, 3.3; 95% CI, 1.3ŌĆō8.6; p=0.020). 53 In a cohort study conducted in the US, among 122,899 people who underwent flexible sigmoidoscopy or colonoscopy between 1989 and 2013, when serrated polyps Ōēź10 mm in size were detected, the risk of CRC incidence increased by 3.35-fold compared to cases without polyps (HR, 3.35; 95% CI, 1.37ŌĆō8.15, p=0.008). 24 In another cohort study conducted from 2004 to 2015 in the US among 5,433 patients, when serrated polyps Ōēź10 mm were detected at index colonoscopy, detection of new serrated polyps Ōēź10 mm in colonoscopic surveillance showed a significant increase compared to the cases without adenomas or serrated polyps at index colonoscopy (OR, 14.34; 95% CI, 5.03ŌĆō40.86). 56 However, in a case-control study conducted from 1998 to 2013 in the US among 2,723 participants, there was no significant difference in future advanced neoplasia incidence between those detected with SSLs Ōēź10 mm and those with SSLs <10 mm (OR, 1.22; 95% CI, 0.29ŌĆō5.10). 73 To summarize the above evidence, shortening of the surveillance period should be considered in patients with serrated polyps Ōēź10 mm at index colonoscopy because of the increased risk of CRC incidence in colonoscopic surveillance. In the 2020 ESGE and BSG guidelines, serrated polyps Ōēź10 mm are classified as high-risk, and colonoscopic surveillance is recommended 3 years after polypectomy. 11,12 The USMSTF guidelines classify serrated polyps into different types; for SSLs Ōēź10 mm, colonoscopic surveillance is recommended after 3 years, whereas for hyperplastic polyps Ōēź10 mm, colonoscopic surveillance is recommended after 3 to 5 years. 10
8) Is the number of SSLs a risk factor that should be considered when shortening the colonoscopic surveillance interval?
Statement 8. Shortening the colonoscopic surveillance interval may be considered depending on the number of lesions for a patient detected with a SSL <10 mm in size at index colonoscopy.
(Strength of Recommendation: Conditional recommendation; Level of Evidence: Very low)
To date, there has been insufficient evidence to clarify whether the risk of developing CRC or advanced neoplasia increases when serrated polyps are removed during index colonoscopy. Recent guidelines state that re-discussion is required on this matter after more research evidence has been gathered. 10,12 According to the USMSTF guidelines published in 2020, for the removal of SSLs <10 mm during index colonoscopy, colonoscopic surveillance should be performed depending on the number of lesions: 5 to 10 years for 1 to 2 lesions, 3 to 5 years for 3 to 4 lesions, and 3 years for 5 to 10 lesions. Additionally, if <20 hyperplastic polyps <10 mm are detected at index colonoscopy, colonoscopic surveillance is recommended after 10 years. 10 Similarly, according to the BSG guidelines, if there are Ōēź5 serrated polyps on index colonoscopy, colonoscopic surveillance is recommended after 3 years. 12 To summarize, this guideline recommends that colonoscopic surveillance intervals according to the number of SSLs at index colonoscopy be considered based on the strategy for the number of adenomas.
9) Is piecemeal resection of colorectal polyps Ōēź20 mm in size a more influential risk factor, than en bloc resection of the polyps, that should be considered when shortening the colonoscopic surveillance interval?
Statement 9. For patients with piecemeal resection of colorectal polyps Ōēź20 mm in size, shortening the colonoscopic surveillance interval should be considered.
(Strength of Recommendation: Strong recommendation; Level of Evidence: Low)
Piecemeal resection of colorectal polyps has a higher rate of incomplete resection than en bloc resection, and is a well-known risk factor for local recurrence after colorectal polyp resection. In a large-scale prospective study of 1,427 patients, the rate of incomplete resection with en bloc resection was reportedly 8.4%, while that with piecemeal resection was considerably higher at 20%. 74 According to a meta-analysis published in 2014, when en bloc resection was performed during endoscopic mucosal resection of non-pedunculated colorectal lesions, the risk of local recurrence was only 3%. However, in cases of piecemeal resection, the risk of recurrence increased to 20%. 75 In particular, the fact that 75% of the local recurrences were detected within 3 months after the procedure indicates the importance of early follow-up in the case of piecemeal resection. 75 According to the results of a large-scale multicenter prospective study by Pellise et al. 76 for serrated lesions Ōēź20 mm published in 2017, the adjusted HR for recurrence of colorectal lesions increased to 3.4 when piecemeal resection was performed compared to en bloc resection (1.0 vs. 3.4, p= 0.002). In cases of piecemeal resection, the degree of recurrence varies depending on the characteristics of the resected lesions and procedure. Tate et al. 77 reported that in the case of piecemeal resection for colorectal polyps, the risk of endoscopically determined recurrence after piecemeal resection increased if the polyp size was >40 mm, bleeding occurred during the procedure, or high-grade dysplasia was present. Another study reported that the average period from resection to recurrence decreased as the number of divided lesions increased during piecemeal resection. 78 However, another recent study reported that the risk of recurrence decreased when additional thermal ablation of the post-EMR mucosal defect margin was performed after piecemeal resection of colorectal polyps. 79 Therefore, In the case of piecemeal resection of colorectal polyps, the operator should pay attention to follow-up in the following situations: (1) if the polyp is large, (2) bleeding occurs during the procedure, and (3) in the presence of high-grade dysplasia. Thus, efforts should be made to minimize the number of divided lesions when performing piecemeal resection. Additionally, various approaches should be developed to reduce the risk of recurrence during piecemeal resections. Based on these studies, most foreign guidelines recommend a short interval of repeat colonoscopy in cases of piecemeal resection of colorectal polyps Ōēź20 mm. The 2020 USMSTF guidelines recommend that in cases of piecemeal resection of adenomas Ōēź20 mm or SSLs Ōēź20 mm, the first colonoscopic surveillance should be conducted within 6 months, the second surveillance should be conducted 1 year after the first, and the third surveillance should be conducted 3 years after the second. 10 The ESGE guidelines published in 2020 also recommend colonoscopic surveillance within 3 to 6 months after piecemeal resection of colorectal polyps Ōēź20 mm, similar to the recommendation of the USMSTF guidelines. 11 However, unlike the 2013 ESGE guidelines, where the reference polyp size was set at 10 mm, the reference size of polyps was increased to Ōēź20 mm according to these guidelines. This is because most studies presented as evidence for the recommendation were conducted with polyps Ōēź20 mm. To summarize, colorectal polyps Ōēź20 mm in size showed an increasing trend in recurrence rate when piecemeal resection was performed compared to en bloc resection. The extent to which piecemeal resection increases the risk of metachronous advanced neoplasia remains unclear. However, considering that colorectal polyps Ōēź20 mm in size increase the risk of CRC in the long term, the risk of advanced neoplasia is predicted to increase at recurrence after piecemeal resection. Therefore, in cases of piecemeal resection of colorectal polyps Ōēź20 mm, colonoscopic surveillance is recommended six months after the procedure.
10) Is a family history of CRC a risk factor that should be considered when shortening the colonoscopic surveillance interval?
Statement 10. Shortening the postpolypectomy colonoscopic surveillance interval is not recommended in patients with a family history of CRC.
(Strength of Recommendation: Conditional recommendation; Level of Evidence: Low)
Several studies have been performed to determine the effect of a family history of CRC on the incidence of advanced adenoma or CRC incidence. In 2015, Jang et al. 80 conducted a retrospective analysis of the results of colonoscopic surveillance of 434 patients who had advanced adenoma removed; however, the family history of CRC did not increase the risk of developing advanced adenoma during surveillance colonoscopies. In 2016, Park et al. 81 performed a retrospective analysis of the results of colonoscopic surveillance in 1,479 patients with advanced adenoma removed in a multi-institutional study with the participation of 13 Korean hospitals. The results showed that the risk of adenoma or CRC incidence (HR, 0.97; 95% CI, 0.69ŌĆō1.38; p=0.883) and the risk of developing advanced adenoma (HR, 0.61; 95% CI, 0.23ŌĆō1.67; p=0.338) showed no statistically significant increase in patients with a family history of CRC than those without. Additionally, in a prospective analysis of eight studies on the risk of advanced adenoma or CRC incidence by conducting colonoscopic surveillance for 9,167 patients with adenomas removed, no significant correlation was observed between the risk of adenoma or advanced adenoma and family history of CRC. 82 In 2018, Jacobs et al. 83 analyzed the results of colonoscopic surveillance of 7,697 patients with adenomas removed from eight studies, which included six RCTs, and the results did not hint at an increased risk of advanced adenoma or CRC in patients with a family history of CRC (OR, 1.15; 95% CI, 0.96ŌĆō1.37). To summarize, most studies that analyzed the relationship between the family history of CRC and risk of developing advanced adenoma or CRC in colonoscopic surveillance after polyp removal did not present a high level of evidence of the correlation, and no statistically significant correlation was observed. Moreover, as most studies either excluded patients with hereditary CRC, such as familial adenomatous polyposis and hereditary non-polyposis CRC (Lynch syndrome), or were not sufficiently large to include these patients, we hereby specify that this statement is not a recommendation for patients with hereditary CRC. If there is a family history of CRC and related tumors, the possibility of hereditary CRC should be carefully examined and a colonoscopic surveillance plan should be established accordingly.
Timing of postpolypectomy surveillance
1) For patients without CRC-related high-risk findings after resecting the polyps, what is the appropriate timing and interval for colonoscopic surveillance?
Statement 11. If there are no high-risk findings related to CRC after complete resection of polyps at high-quality index colonoscopy performed with adequate bowel preparation, colonoscopic surveillance after 5 to 10 years from polypectomy is recommended. However, if the above prerequisites are not satisfied or a high-risk finding of CRC incidence is detected after polypectomy before conducting index colonoscopy, the surveillance interval can be shortened even if no high-risk finding is detected at index colonoscopy.
(Strength of Recommendation: Strong recommendation; Level of Evidence: Moderate)
In the 2012 Korean guidelines, following a systematic literature search and meta-analysis, an increased risk of developing advanced neoplasia was considered when at least one of the following findings was observed at index colonoscopy after polypectomy, and the cases were defined as having a high-risk finding: Ōēź3 adenomas, adenomas Ōēź10 mm in size, tubulovillous or villous adenoma, adenoma with high-grade dysplasia, and serrated polyp Ōēź10 mm in size. 9 In 2007, Lieberman et al. 84 reported that in a case of <3 tubular adenomas <10 mm at index colonoscopy, the incidence of advanced neoplasia within 5.5 years of the surveillance interval was 4.6%, indicating a higher RR of 1.92 (95% CI, 0.83ŌĆō4.42) compared to the controls without adenomas; however, the difference was not statistically significant. Compared with controls, however, there was a significant increase in the risk of advanced neoplasia incidence at 11.9% (RR, 5.01; 95% CI, 2.10ŌĆō11.96) in the case of Ōēź3 adenomas <10 mm, 15.5% (RR, 6.40; 95% CI, 2.74ŌĆō14.94) for adenomas Ōēź10 mm, 16.1% (RR, 6.05; 95% CI, 2.48ŌĆō14.71) for villous adenoma, and 17.4% (RR, 6.87; 95% CI, 4.61ŌĆō18.07) for adenomas with high-grade dysplasia. In a single prospective cohort study conducted in Korea published in 2011 for 3,803 asymptomatic patients aged 50 to 69 years, when <3 adenomas <10 mm were detected at index colonoscopy, the 5-year cumulative incidence of advanced neoplasia showed no significant difference (2.4% vs. 2.0%; HR, 1.14; 95% CI, 0.61ŌĆō2.17) over controls. However, for adenomas Ōēź10 mm, Ōēź3 adenomas, villous adenomas, or adenomas with high-grade dysplasia, the 5-year cumulative incidence of advanced neoplasia was high at 12.2% and the advanced neoplasia developed within 3 to 4 years in most cases. 85 Considered together, The previous guidelines recommended a surveillance interval of 5 years for cases without high-risk findings of advanced neoplasia at index colonoscopy by differentiating from cases with high-risk findings, but the level of evidence was low. In many cohort studies conducted since 2012, the risk of CRC incidence and mortality in cases of adenomas without high-risk findings after polypectomy was similar to the normal findings at index colonoscopy. 24,28,36,86 In 2018, Click et al. 28 performed a post-hoc analysis of RCT results on the effect of CRC screening with flexible sigmoidoscopy conducted since 1993. They reported that in the case of adenomas <10 mm without villous adenoma or high-grade dysplasia, there was no significant difference in the risk of developing CRC within 15 years compared to those without adenomas (RR, 1.2; 95% CI, 0.8ŌĆō1.7; p=0.300). In 2020, He et al. 24 also reported that in the case of adenomas <10 mm in size without villous adenoma or high-grade dysplasia (HR, 1.21; 95% CI, 0.68ŌĆō2.16; p=0.520) and serrated lesions <10 mm (HR, 1.25; 95% CI, 0.76ŌĆō2.08; p=0.380), there was no significant difference in the risk of 10-year CRC incidence compared to the controls without polyps. In some studies, the risk of CRC incidence and mortality was significantly reduced in the case of adenomas without a high-risk finding after polypectomy at index colonoscopy compared with the general population. This is thought to be because endoscopic resection of adenomas without high-risk findings detected at index colonoscopy contributes to preventing CRC morbidity and mortality. 5,22,87 Additionally, a retrospective cohort study published by He et al. 24 in 2020 reported that adenomas <10 mm in size without villous adenoma or high-grade dysplasia and serrated lesions <10 mm showed no increased risk of 10-year CRC incidence compared with controls without polyps, regardless of the status or number of surveillance colonoscopies. Therefore, there is an increasing body of evidence in recent studies suggesting that surveillance colonoscopy has no additional effect on reducing CRC incidence when there are no CRC-related high-risk findings after polypectomy. Meta-analyses have reported that the incidence of advanced neoplasia in colonoscopic surveillance conducted within five years is higher for adenomas without high-risk findings at index colonoscopy than in the normal group; however, the results also include those without statistical significance. 88,89
Individuals without CRC-related high-risk findings after polypectomy are deemed to have the same risk level as that of the normal group in terms of CRC incidence, suggesting that the same colonoscopic surveillance interval could be set for the normal group. Considering that the main purpose of colonoscopic surveillance is to reduce CRC incidence and mortality, this point should be considered a clear guideline. A colonoscopic surveillance interval of 10 years is generally recommended for the normal group. 10 Therefore, colonoscopic surveillance may be recommended 10 years after polypectomy for individuals with no CRC-related high-risk findings. However, the prerequisite to this recommendation is the complete resection of polyps at high-quality index colonoscopy conducted under adequate bowel preparation. In Korea, considering the relatively low medical costs and high accessibility of healthcare services, the 5-year interval, according to previous guidelines, can serve as an alternative for the transition period to some extent. In the future, if more data on colonoscopic surveillance at 10-year intervals are gathered, the 10-year interval may be established as a recommendation for individuals with no CRC-related high-risk findings following polypectomy. Therefore, colonoscopic surveillance should be conducted 5 to 10 years after polypectomy if there are no high-risk findings related to CRC at the index colonoscopy.
2) For patients with CRC-related high-risk findings after resection of polyps, what is the appropriate timing and interval for colonoscopic surveillance?
Statement 12. In the case of CRC-related high-risk findings after polypectomy in high-quality index colonoscopy (adenoma Ōēź10 mm, 3 to 5 or more adenomas, tubulovillous adenoma or villous adenoma, adenoma with high-grade dysplasia, TSA, SSL with dysplasia, serrated polyp Ōēź10 mm, 3 to 5 or more SSLs), shortening of the colonoscopic surveillance interval should be considered by analyzing the specifics of each situation. However, in the case when the above prerequisites have not been satisfied or considering the colonoscopy findings prior to index colonoscopy, the status of adenoma resection, systemic condition of the patient, family history, and medical history of the patient, the surveillance interval can be further adjusted.
(Strength of Recommendation: Strong recommendation; Level of Evidence: Moderate)
In cases of CRC-related high-risk findings after polypectomy at index colonoscopy, the colonoscopic surveillance interval should be shortened, and such high-risk findings can be determined based on the size, number, and histological findings of the resected polyps. In this guideline, the colonoscopic surveillance interval is presented in Table 4 and Figure 1 according to specific situations. In a large-scale prospective US cohort study with 15,935 patients detected with polyps at index colonoscopy, the risk of CRC incidence in patients with advanced neoplasia was 13% higher than in those without. 28 In another large cohort study in the US of 3,300 patients, for a high-risk group with adenomas Ōēź10 mm in size, the risk of advanced neoplasia incidence increased by 3.6-fold (OR, 3.6; 95% CI, 2.8ŌĆō4.5), and by 5.2-fold for CRC incidence (OR, 5.2; 95% CI, 1.8ŌĆō15.1) in colonoscopic surveillance. 44 In a large prospective cohort study conducted in Poland that enrolled 236,089 patients with polyps detected at index colonoscopy, the SIR of CRC increased in high-risk groups with the polyps Ōēź20 mm in size (2.07; 95% CI, 1.40ŌĆō2.93) or adenomas with high-grade dysplasia (0.79; 95% CI, 0.39ŌĆō1.41). 22 According to a multi-institutional prospective study in Korea conducted with 372 patients, the risk of developing advanced neoplasia during colonoscopic surveillance increased by 2.37-fold (OR, 2.37; 95% CI, 1.55ŌĆō3.63) in the high-risk group with tubulovillous adenoma or villous adenoma at index colonoscopy. 60 According to a cohort study conducted in the US of 5,433 patients, those detected with serrated polyps Ōēź10 mm at index colonoscopy had a 14.34-fold increase in the risk of serrated polyps Ōēź10 mm in colonoscopic surveillance (OR, 14.34; 95% CI, 5.03ŌĆō40.86). However, the risk of developing advanced neoplasia in colonoscopic surveillance did not increase significantly. 56 When the number of adenomas was Ōēź3 at index colonoscopy, the risk of advanced neoplasia incidence increased by 1.61-fold (OR, 1.61; 95% CI, 1.46ŌĆō1.78), and the risk of CRC by 4.3-fold (OR, 4.3; 95% CI, 1.40ŌĆō12.90). 12,44 Additionally, when there were 1ŌĆō2 and 3ŌĆō4 adenomas <10 mm, the incidence of advanced neoplasia in colonoscopic surveillance was similar at 1.4% and 1.8%, respectively, whereas in the case of Ōēź5 adenomas <10 mm, the advanced neoplasia incidence was 5%. This indicates that with an increase in the number of adenomas, there is a significant increase in the risk of developing advanced neoplasia. 29 Therefore, in cases with high-risk findings of advanced neoplasia at index colonoscopy, colonoscopic surveillance is needed to detect advanced neoplasia and reduce CRC incidence and mortality. Most high-quality studies related to the risk factors for advanced neoplasia incidence are follow-up studies conducted with a cohort of participants in polyp prevention trials. These studies were conducted after the National Polyp Study, and surveillance was performed after index colonoscopy. In these studies, the risk of advanced adenoma increased in the high-risk group in surveillance conducted 3 years after index colonoscopy; however, the actual CRC incidence was rare. Thus, based on the evidence, adequate timing of surveillance for the high-risk group may be recommended as 3 years. Recent studies have compared the colonoscopic surveillance interval of 3 years to intervals within 3 years. In the case of surveillance interval of 3 years, although the incidence of advanced adenoma was high (OR, 2.02; 95% CI, 1.19ŌĆō3.42), there was no significant difference in terms of CRC incidence and mortality; thus, the appropriate colonoscopic surveillance interval for high-risk groups may be recommended as 3 years. 21,90 However, in many cases, patients who participated in the National Polyp Study and other clinical studies underwent high-quality examination by colonoscopists. Those who had complete resection of the polyps examined before inclusion in the study underwent a clearing colonoscopy to remove missed polyps. Moreover, considering that many studies excluded patients with a family history of CRC, it is recommended that in determining surveillance timing in clinical practice, in addition to the number or size of adenomas, histological features, and distribution observed at index colonoscopy, detailed information on the quality of colonoscopy examination, family history of CRC, and medical history should also be considered. Another point to consider is that when the examination of patients shows two or more findings among the findings corresponding to the high-risk group that increases the risk of detection of CRC or advanced neoplasia in postpolypectomy colonoscopic surveillance, a few studies have examined whether such cases with multiple findings increase the level of risk. According to a study by Atkin et al. 91 in 1992 using rectosigmoidoscopy, in the high-risk group that had villous adenoma/tubulovillous adenoma or adenomas Ōēź10 mm in size at the baseline examination, the SIR of CRC for the group with one adenoma was 2.9 (95% CI, 1.80ŌĆō4.50), and for the group with two or more adenomas, the CRC SIR increased to 6.6 (95% CI, 3.30ŌĆō11.80). In 2000, Noshirwani et al. 92 reported that if there were three adenomas <10 mm in size at index colonoscopy, the risk of developing advanced adenoma was estimated to be 8.5% in the surveillance conducted after 42 months, and for cases of Ōēź3 adenomas with the largest of them was Ōēź10 mm, the risk increased to 21.3%. Additionally, if there were Ōēź4 adenomas <10 mm in size, the risk of developing advanced adenoma was estimated to be 15.3% in the surveillance, and for cases of Ōēź4 adenomas, with the largest being Ōēź 10 mm, the risk increased up to 34.5%. According to a study by Anderson et al. 56 in 2018 using colonoscopy, the risk of detecting advanced adenoma in colonoscopic surveillance was 3.86 (95% CI, 2.77ŌĆō5.39) in the group that had only adenomas with high-grade dysplasia at the baseline examination; however, for the group with both the adenomas with high-grade dysplasia and serrated lesions, the risk increased to 16.04 (95% CI, 6.95ŌĆō37.00). In a Korean study, the risk of finding advanced adenoma in the surveillance conducted after 3 years was estimated to be 10.7% in the group that was detected to have only adenomas at index colonoscopy, while the risk increased to 17.9% when both adenomas and serrated lesions were detected. 93 These findings indicate that the risk of advanced neoplasia increases if the patient has multiple findings that correspond to the high-risk group. Based on this evidence, if there are two or more findings corresponding to the high-risk group, there is a possibility that the surveillance interval should be shortened. However, owing to the lack of research in these areas, it is challenging to recommend a clear guideline for surveillance intervals.
DISCUSSION
Patients with removed colorectal polyps have an increased risk of developing colorectal polyps or neoplasia in the future; therefore, management based on appropriate colonoscopic surveillance is required. 4,5 This is a well-established fact over time, and appropriate colonoscopic surveillance is essential for establishing a long-term CRC prevention strategy. To this end, many medical societies in Korea and abroad have developed and distributed guidelines for postpolypectomy colonoscopic surveillance. Since 2020, the USMSTF, ESGE, and BSG have updated these guidelines. In line with these changes, the Guidelines Development Committee of Korea presents the interval of postpolypectomy colonoscopic surveillance for Korean patients with colorectal polyps based on a literature review. At index colonoscopy, if the patient is diagnosed with at least one of the following, the patient is classified into the high-risk group with an increased risk of future CRC incidence: (1) adenoma Ōēź10 mm, (2) 3 to 5 or more adenomas, (3) tubulovillous adenoma or villous adenoma, (4) adenoma with high-grade dysplasia, (5) TSA, (6) SSL with dysplasia, (7) serrated polyp Ōēź10 mm, and (8) 3 to 5 or more SSLs. For the above high-risk groups, we recommend shortening the interval of postpolypectomy colonoscopic surveillance; for those without the specified high-risk polypectomy findings, colonoscopic surveillance should be conducted 5 to 10 years after polypectomy. Adequate bowel preparation and high-quality examination are among the most important factors in establishing an appropriate interval for colonoscopic surveillance. Therefore, in the case of this guideline, unlike previous guidelines, the definitions of adequate bowel preparation and high-quality examination were specified in detail in the guideline development process. In cases of inadequate examination during index colonoscopy, subsequent colonoscopic surveillance may be needed to complement the initial inadequate examination, which is a significant limitation. According to a large cohort study, an inadequate level of colonoscopy examination at baseline increased the risk of CRC incidence and mortality after polypectomy, regardless of colonoscopic surveillance. 21 Inadequate bowel preparation also increases the colonoscopic miss rate of colorectal polyps. Accordingly, most guidelines recommend that the postpolypectomy colonoscopic surveillance interval should be applied to patients with adequate bowel preparation. 94 Therefore, adequate bowel preparation and high-quality examinations in clinical practice are crucial, and both must be checked as prerequisites before colonoscopic surveillance. According to the present guidelines, the risk of advanced neoplasia and CRC incidence increased during colonoscopy surveillance when the number of adenomas at index colonoscopy was 3 to 5 or more. This was confirmed based on the meta-analysis reviewed when preparing the present guidelines as well as the recently revised USMSTF guidelines. As discussed previously, according to the meta-analysis, there was a statistically significant increase in the RR of developing advanced neoplasia in the group that had 3 to 5 or more adenomas removed compared to the group with 1 to 2 adenomas removed. Furthermore, the RR of CRC incidence increased with the number of adenomas, although the increase was not statistically significant. Therefore, in terms of determining the risk of future CRC and advanced neoplasia for evaluating the present guidelines, it was determined that there was a risk of 3 to 5 adenomas or more. The USMSTF guidelines also recommend colonoscopic surveillance 3 to 5 years after the development of Ōēź3 adenomas, although the surveillance interval is slightly longer than in previous guidelines. 10 However, in the BSG and ESGE guidelines, if the number of adenomas is Ōēź5, the case is considered high-risk. 11,12 This is thought to reflect the results of recently published studies showing that the risk of advanced neoplasia did not significantly increase when the number of adenomas was <5. 21,28 As more research evidence is gathered in the future, the colonoscopic surveillance interval may change according to the number of adenomas. A serrated polyp in the colon is an umbrella term used to describe hyperplastic polyps, SSLs, and TSA based on pathological diagnostic criteria. 95 Serrated polyps cause CRC through the serrated pathway rather than carcinogenesis by general adenomas and are currently recognized as important risk factors for CRC and interval CRC. 56,96,97 Therefore, recent international guidelines have added more content to colonoscopic surveillance of these serrated polyps. In the ESGE guidelines published in 2013, there was no recommendation regarding serrated polyps. However, in the revised guidelines of 2020, if the size of the serrated polyps is Ōēź10 mm or if it contains dysplasia, colonoscopic surveillance is recommended after three years. 11 The BSG guidelines published in 2020 also specify serrated polyps as premalignant. 12 However, small (1ŌĆō5 mm) hyperplastic polyps in the rectum were excluded from the classification. In the case of the USMSTF guidelines, categorized repeat colonoscopy intervals are presented for serrated polyps, and the interval is set similar to the surveillance interval for adenomas in general. 10 For SSLs Ōēź10 mm or those containing dysplasia, the recommended colonoscopic surveillance interval is 3 years. Similarly, when the number of detected SSLs is 5 to 10 or if it contains TSA, it is recommended to conduct colonoscopic surveillance after 3 years. In the case of the present Korean guidelines, adding to the recommendation of previous guidelines in which only serrated polyps Ōēź10 mm are classified as high-risk, SSLs with dysplasia, 3 to 5 or more SSLs, or detection of TSA are also categorized as high-risk. Based on these findings, colonoscopic surveillance after 3 years is recommended. This revised edition of the Korean guidelines contains new additions compared to previous guidelines as well as parts that are not specifically stated, as in the case of previous guidelines. Piecemeal resection of colorectal polyps is a new addition to this revision. The guidelines published in 2012 had no recommendation on the colonoscopic surveillance interval for piecemeal resection of colorectal polyps. 9 This is because there have been only a few relevant studies in the past, and there is insufficient evidence to recommend a specific colonoscopic surveillance interval. Many studies on the development of metachronous colorectal neoplasia at piecemeal resection were published after 2012. 74-76 In line with the research evidence, foreign guidelines revised in 2020 all contain recommendations for conducting colonoscopic surveillance 3 to 6 months after piecemeal resection of colorectal polyps Ōēź20 mm. 10-12 In this revised edition of the guidelines, considering the results of more studies gathered to date and overseas guidelines, although the level of evidence is low, it was judged that the risk of metachronous advanced neoplasia increases in the case of piecemeal resection of colorectal polyps Ōēź20 mm; therefore, conducting colonoscopic surveillance after six months is recommended. Unlike piecemeal resection, the revised guidelines do not present a separate timing for the second colonoscopic surveillance, as in the previous guidelines. This is because there is a lack of evidence in terms of research on second colonoscopic surveillance and foreign guidelines also show differences and inconsistencies in their recommendations. Additionally, given the high level of accessibility to colonoscopy in Korea, it is difficult to present specific recommendations for a second colonoscopic surveillance at this point. The age at which postpolypectomy colonoscopic surveillance is stopped differs slightly depending on the guidelines; in most cases, the recommended age is 75 to 80 years. 11,12 However, research on elderly patients regarding the age at which postpolypectomy colonoscopic surveillance is stopped has provided insufficient evidence. Since this issue is highly dependent on the accessibility of medical resources in each country, as well as the health condition of individual patients, there is a limit to applying uniform criteria for all patients. Moreover, since complications from colonoscopy show an increasing trend in the elderly, careful weighing of the possible harm caused by colonoscopy surveillance is important. 98,99 Therefore, the judgment of individual physicians considering the various factors described above is thought to be important in clinical practice, and it is necessary to provide proper explanations regarding the benefits and harms of colonoscopy surveillance for elderly patients.
CONCLUSIONS
This guideline is a revision of the guidelines published in 2012, and is the second version in Korea. Although some studies on postpolypectomy colonoscopic surveillance have been conducted in Korea since 2012, available data are still limited. In Western countries, the healthcare environment is fundamentally different from that of Korea; in particular, there are considerable differences in terms of examination cost and access to colonoscopy. Guidelines greatly influence the clinical practice of physicians, and the scope of the influence is not limited to individual physicians, but affects the entire country beyond local communities. Therefore, for the Korean guidelines, the utility of medical resources should be considered in the future, and a cost-effectiveness analysis should be performed as a starting point. A cost-effectiveness analysis should be conducted based on research data in Korea, in accordance with the domestic healthcare environment, and if necessary, a comparative analysis with other countries should be conducted. The present guidelines are expected to help physicians to select more efficient and optimal methods for treating patients in real-world clinical settings. The last point to mention is that since there is a practical limitation to making decisions based only on guidelines considering clinical information of individual patients and various situations, the clinical judgment of individual physicians about the surveillance method and timing derived by synthesizing the guidelines and using various clinical data is thought to be the most important.
Appendix
Appendix 4. Schema illustrating the flow of the search and selection of literature for development of the guidelines for post-polypectomy colonoscopic surveillance.
Supplementary Material
Supplementary Fig. 1. The incidence and relative risk of metachronous colorectal advanced neoplasia in the meta-analysis.
Supplementary Fig. 2. The incidence and relative risk of metachronous colorectal cancer in the meta-analysis.
Supplementary Table 1. The incidence of metachronous advanced neoplasia according to the number of non-advanced colorectal adenoma.
Supplementary Table 2. The relative risk of metachronous advanced neoplasia according to the number of non-advanced colorectal adenoma.
Fig.┬Ā1.
Recommendations for postpolypectomy colonoscopic surveillance. 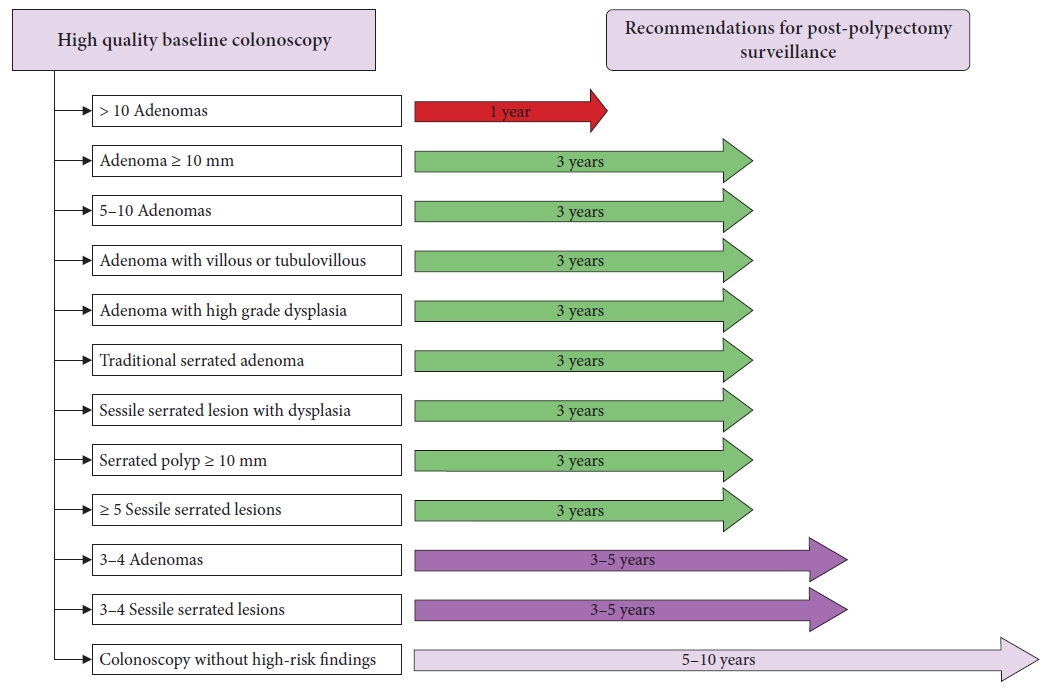
Table┬Ā1.
Definition of level of evidence
|
Level of evidence |
Definition |
|
High |
ßø½ Study design: |
|
Intervention: The results are derived from randomized controlled trials (RCTs) or observational studies with control groups. |
|
Diagnosis: Diagnostic accuracy studies in the form of RCTs or cross-sectional cohort studies |
|
ßø½ Considerations: There are no methodological concerns in terms of quality assessment of the evidence, and the evidence shows consistency with a sufficient level of precision; thus, the reliability of the synthesized results is considered high. |
|
Moderate |
ßø½ Study design: |
|
Intervention: The results are derived from RCTs or observational studies with control groups. |
|
Diagnosis: Diagnostic accuracy studies in the form of RCTs or cross-sectional cohort studies |
|
ßø½ Considerations: There are slight concerns regarding the quality assessment, consistency, or precision of the evidence; thus, the reliability of the synthesized result is considered moderate. |
|
Low |
ßø½ Study design: |
|
Intervention: Results are derived from observational studies with or without controls/comparators. |
|
Diagnosis: Diagnostic accuracy studies with a case-control design |
|
ßø½ Considerations: |
|
There are serious concerns regarding the quality assessment, consistency, or precision of the evidence; thus, the reliability of the synthesized result is considered low. |
|
Very low |
ßø½ Study design: |
|
Intervention: Observational studies without controls/comparators or studies consisting of evidence-based on expert opinions or reviews |
|
Diagnosis: Diagnostic accuracy studies with a case-control design |
|
ßø½ Considerations: There are critical concerns regarding the quality assessment, consistency, or precision of the evidence; thus, the reliability of the synthesized result is considered very low. |
Table┬Ā2.
Definition of strength of recommendation
|
Symbol |
Strength of recommendation |
Description |
|
A |
Strong recommendation |
Considering the benefits and harms, level of evidence, values and preferences, as well as resources of the intervention/examination, it is strongly recommended in most clinical situations. |
|
B |
Conditional recommendation |
Considering that the use of the intervention/examination may vary depending on the clinical situation or values of the patient/society, selective use or conditional selection of the intervention/examination is recommended. |
|
C |
Not recommended |
The harm of the intervention/examination may outweigh the benefits, and considering the clinical situations or values of the patients/society, the use of the intervention/examination is not recommended. |
|
I |
Inconclusive |
Considering the benefit and harm, level of evidence, values and preferences, as well as resources required for the intervention/examination, the level of evidence is too low, the weighing of the benefit/harm is seriously indecisive, or the variability is large. Therefore, the use of the intervention/examination is not determined. |
Table┬Ā3.
Key questions addressed in this study
|
ŌĆā |
|
Key question 1. Is the size of the tubular adenoma a risk factor that should be considered when shortening the colonoscopic surveillance interval? |
|
Key question 2. Is the number of colorectal adenomas a risk factor that should be considered when shortening the colonoscopic surveillance interval? |
|
Key question 3. Is a tubulovillous or villous adenoma a more influential risk factor that should be considered when shortening the colonoscopic surveillance interval compared to a tubular adenoma? |
|
Key question 4. Is a serrated polyp a risk factor that should be considered when shortening the colonoscopic surveillance interval? |
|
Key question 5. Is a traditional serrated adenoma a risk factor that should be considered when shortening the colonoscopic surveillance interval? |
|
Key question 6. Is histology of sessile serrated lesion with dysplasia a risk factor that should be considered when shortening the colonoscopic surveillance interval? |
|
Key question 7. Is the size of a serrated polyp a risk factor that should be considered when shortening the colonoscopic surveillance interval? |
|
Key question 8. Is the number of sessile serrated lesions a risk factor that should be considered when shortening the colonoscopic surveillance interval? |
|
Key question 9. Is piecemeal resection of colorectal polyps Ōēź20 mm in size a more influential risk factor, than en bloc resection of the polyps, that should be considered when shortening the colonoscopic surveillance interval? |
|
Key question 10. Is a family history of colorectal cancer a risk factor that should be considered when shortening the colonoscopic surveillance interval? |
|
Key question 11. For patients without colorectal cancer-related high-risk findings after resection of polyps, what is the appropriate timing and interval for colonoscopic surveillance? |
|
Key question 12. For patients with colorectal cancer-related high-risk findings after resection of polyps, what is the appropriate timing and interval for colonoscopic surveillance? |
Table┬Ā4.
Summary and strength of recommendations for postpolypectomy colonoscopic surveillance
|
Index colonoscopy finding |
Interval of colonoscopic surveillance |
Strength of recommendation |
Level of evidence |
|
Adenoma Ōēź10 mm in size |
3 yr |
Conditional recommendation |
Low |
|
3ŌĆō4 adenomasa)
|
3ŌĆō5 yr |
Conditional recommendation |
Moderate |
|
5ŌĆō10 adenomasa)
|
3 yr |
Conditional recommendation |
Moderate |
|
|
|
|
|
Number of adenomas >10a)
|
1 yr |
Conditional recommendation |
Moderate |
|
|
|
|
|
Tubulovillous adenoma or villous adenoma |
3 yr |
Strong recommendation |
Low |
|
Adenoma with high-grade dysplasia |
3 yr |
Strong recommendation |
Moderate |
|
Traditional serrated adenoma |
3 yr |
Conditional recommendation |
Low |
|
Sessile serrated lesion with dysplasia |
3 yr |
Conditional recommendation |
Very low |
|
Serrated polyp Ōēź10 mm |
3 yr |
Conditional recommendation |
Very low |
|
No. of sessile serrated lesions between 3ŌĆō4b)
|
3ŌĆō5 yr |
Conditional recommendation |
Very low |
|
No. of sessile serrated lesions Ōēź5b)
|
3 yr |
Conditional recommendation |
Very low |
|
Piecemeal resection of colorectal polyps Ōēź20 mm in size |
6 mo |
Strong recommendation |
Low |
REFERENCES
2. Winawer SJ, Zauber AG, Ho MN, et al. Prevention of colorectal cancer by colonoscopic polypectomy: the National Polyp Study Workgroup. N Engl J Med 1993;329:1977ŌĆō1981.   4. Robertson DJ, Greenberg ER, Beach M, et al. Colorectal cancer in patients under close colonoscopic surveillance. Gastroenterology 2005;129:34ŌĆō41.   5. Cottet V, Jooste V, Fournel I, et al. Long-term risk of colorectal cancer after adenoma removal: a population-based cohort study. Gut 2012;61:1180ŌĆō1186.   9. Hong SN, Yang DH, Kim YH, et al. Korean guidelines for post-polypectomy colonoscopic surveillance. Korean J Gastroenterol 2012;59:99ŌĆō117.   11. Hassan C, Antonelli G, Dumonceau JM, et al. Post-polypectomy colonoscopy surveillance: European Society of Gastrointestinal Endoscopy (ESGE) Guideline: update 2020. Endoscopy 2020;52:687ŌĆō700.   16. Mustafa RA, Santesso N, Brozek J, et al. The GRADE approach is reproducible in assessing the quality of evidence of quantitative evidence syntheses. J Clin Epidemiol 2013;66:736ŌĆō742.   17. Zhang Y, Akl EA, Sch├╝nemann HJ. Using systematic reviews in guideline development: the GRADE approach. Res Synth Methods 2019;10:312ŌĆō329.   18. Kaminski MF, Thomas-Gibson S, Bugajski M, et al. Performance measures for lower gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement Initiative. Endoscopy 2017;49:378ŌĆō397.   20. Rex DK, Schoenfeld PS, Cohen J, et al. Quality indicators for colonoscopy. Gastrointest Endosc 2015;81:31ŌĆō53.   22. Wieszczy P, Kaminski MF, Franczyk R, et al. Colorectal cancer incidence and mortality after removal of adenomas during screening colonoscopies. Gastroenterology 2020;158:875ŌĆō883.   27. Hartstein JD, Vemulapalli KC, Rex DK. The predictive value of small versus diminutive adenomas for subsequent advanced neoplasia. Gastrointest Endosc 2020;91:614ŌĆō621.   29. Vemulapalli KC, Rex DK. Risk of advanced lesions at first follow-up colonoscopy in high-risk groups as defined by the United Kingdom post-polypectomy surveillance guideline: data from a single U.S. center. Gastrointest Endosc 2014;80:299ŌĆō306.   30. Cubiella J, Carballo F, Portillo I, et al. Incidence of advanced neoplasia during surveillance in high- and intermediate-risk groups of the European colorectal cancer screening guidelines. Endoscopy 2016;48:995ŌĆō1002.   31. Laish I, Seregeev I, Naftali T, et al. Surveillance after positive colonoscopy based on adenoma characteristics. Dig Liver Dis 2017;49:1115ŌĆō1120.   33. Moon CM, Jung SA, Eun CS, et al. The effect of small or diminutive adenomas at baseline colonoscopy on the risk of developing metachronous advanced colorectal neoplasia: KASID multicenter study. Dig Liver Dis 2018;50:847ŌĆō852.   34. Park SK, Yang HJ, Jung YS, et al. Risk of advanced colorectal neoplasm by the proposed combined United States and United Kingdom risk stratification guidelines. Gastrointest Endosc 2018;87:800ŌĆō808.   35. Kim NH, Jung YS, Lee MY, et al. Risk of developing metachronous advanced colorectal neoplasia after polypectomy in patients with multiple diminutive or small adenomas. Am J Gastroenterol 2019;114:1657ŌĆō1664.   36. Lieberman D, Sullivan BA, Hauser ER, et al. Baseline colonoscopy findings associated with 10-year outcomes in a screening cohort undergoing colonoscopy surveillance. Gastroenterology 2020;158:862ŌĆō874.   42. Provenzale D, Gupta S, Ahnen DJ, et al. Genetic/familial high-risk assessment: colorectal version 1.2016, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 2016;14:1010ŌĆō1030.   45. van Heijningen EM, Lansdorp-Vogelaar I, Kuipers EJ, et al. Features of adenoma and colonoscopy associated with recurrent colorectal neoplasia based on a large community-based study. Gastroenterology 2013;144:1410ŌĆō1418.   47. Saini SD, Kim HM, Schoenfeld P. Incidence of advanced adenomas at surveillance colonoscopy in patients with a personal history of colon adenomas: a meta-analysis and systematic review. Gastrointest Endosc 2006;64:614ŌĆō626.   48. Mahajan D, Downs-Kelly E, Liu X, et al. Reproducibility of the villous component and high-grade dysplasia in colorectal adenomas <1 cm: implications for endoscopic surveillance. Am J Surg Pathol 2013;37:427ŌĆō433.   49. Foss FA, Milkins S, McGregor AH. Inter-observer variability in the histological assessment of colorectal polyps detected through the NHS Bowel Cancer Screening Programme. Histopathology 2012;61:47ŌĆō52.   51. Macaron C, Vu HT, Lopez R, et al. Risk of metachronous polyps in individuals with serrated polyps. Dis Colon Rectum 2015;58:762ŌĆō768.   52. Erichsen R, Baron JA, Hamilton-Dutoit SJ, et al. Increased risk of colorectal cancer development among patients with serrated polyps. Gastroenterology 2016;150:895ŌĆō902.   53. Holme ├ś, Bretthauer M, Eide TJ, et al. Long-term risk of colorectal cancer in individuals with serrated polyps. Gut 2015;64:929ŌĆō936.   54. Lu FI, van Niekerk de W, Owen D, et al. Longitudinal outcome study of sessile serrated adenomas of the colorectum: an increased risk for subsequent right-sided colorectal carcinoma. Am J Surg Pathol 2010;34:927ŌĆō934.   57. Teriaky A, Driman DK, Chande N. Outcomes of a 5-year follow-up of patients with sessile serrated adenomas. Scand J Gastroenterol 2012;47:178ŌĆō183.   58. Schreiner MA, Weiss DG, Lieberman DA. Proximal and large hyperplastic and nondysplastic serrated polyps detected by colonoscopy are associated with neoplasia. Gastroenterology 2010;139:1497ŌĆō1502.   59. Lazarus R, Junttila OE, Karttunen TJ, et al. The risk of metachronous neoplasia in patients with serrated adenoma. Am J Clin Pathol 2005;123:349ŌĆō359.   60. Yoon JY, Kim HT, Hong SP, et al. High-risk metachronous polyps are more frequent in patients with traditional serrated adenomas than in patients with conventional adenomas: a multicenter prospective study. Gastrointest Endosc 2015;82:1087ŌĆō1093.   61. Payne SR, Church TR, Wandell M, et al. Endoscopic detection of proximal serrated lesions and pathologic identification of sessile serrated adenomas/polyps vary on the basis of center. Clin Gastroenterol Hepatol 2014;12:1119ŌĆō1126.   64. Wong NA, Hunt LP, Novelli MR, et al. Observer agreement in the diagnosis of serrated polyps of the large bowel. Histopathology 2009;55:63ŌĆō66.   65. Bustamante-Bal├®n M, Bernet L, Cano R, et al. Assessing the reproducibility of the microscopic diagnosis of sessile serrated adenoma of the colon. Rev Esp Enferm Dig 2009;101:258ŌĆō264.   66. Farris AB, Misdraji J, Srivastava A, et al. Sessile serrated adenoma: challenging discrimination from other serrated colonic polyps. Am J Surg Pathol 2008;32:30ŌĆō35.   67. Hiraoka S, Kato J, Fujiki S, et al. The presence of large serrated polyps increases risk for colorectal cancer. Gastroenterology 2010;139:1503ŌĆō1510.   68. Lash RH, Genta RM, Schuler CM. Sessile serrated adenomas: prevalence of dysplasia and carcinoma in 2139 patients. J Clin Pathol 2010;63:681ŌĆō686.   69. Imperiale TF, Glowinski EA, Lin-Cooper C, et al. Five-year risk of colorectal neoplasia after negative screening colonoscopy. N Engl J Med 2008;359:1218ŌĆō1224.   70. Lieberman DA, Rex DK, Winawer SJ, et al. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology 2012;143:844ŌĆō857.   74. Pohl H, Srivastava A, Bensen SP, et al. Incomplete polyp resection during colonoscopy-results of the complete adenoma resection (CARE) study. Gastroenterology 2013;144:74ŌĆō80.   75. Belderbos TD, Leenders M, Moons LM, et al. Local recurrence after endoscopic mucosal resection of nonpedunculated colorectal lesions: systematic review and meta-analysis. Endoscopy 2014;46:388ŌĆō402.   76. Pellise M, Burgess NG, Tutticci N, et al. Endoscopic mucosal resection for large serrated lesions in comparison with adenomas: a prospective multicentre study of 2000 lesions. Gut 2017;66:644ŌĆō653.   77. Tate DJ, Desomer L, Klein A, et al. Adenoma recurrence after piecemeal colonic EMR is predictable: the Sydney EMR recurrence tool. Gastrointest Endosc 2017;85:647ŌĆō656.   79. Klein A, Tate DJ, Jayasekeran V, et al. Thermal ablation of mucosal defect margins reduces adenoma recurrence after colonic endoscopic mucosal resection. Gastroenterology 2019;156:604ŌĆō613.   84. Lieberman DA, Weiss DG, Harford WV, et al. Five-year colon surveillance after screening colonoscopy. Gastroenterology 2007;133:1077ŌĆō1085.   85. Chung SJ, Kim YS, Yang SY, et al. Five-year risk for advanced colorectal neoplasia after initial colonoscopy according to the baseline risk stratification: a prospective study in 2452 asymptomatic Koreans. Gut 2011;60:1537ŌĆō1543.   87. L├Ėberg M, Kalager M, Holme ├ś, et al. Long-term colorectal-cancer mortality after adenoma removal. N Engl J Med 2014;371:799ŌĆō807.   88. Hassan C, Gimeno-Garc├Ła A, Kalager M, et al. Systematic review with meta-analysis: the incidence of advanced neoplasia after polypectomy in patients with and without low-risk adenomas. Aliment Pharmacol Ther 2014;39:905ŌĆō912.   89. Dub├® C, Yakubu M, McCurdy BR, et al. Risk of advanced adenoma, colorectal cancer, and colorectal cancer mortality in people with low-risk adenomas at baseline colonoscopy: a systematic review and meta-analysis. Am J Gastroenterol 2017;112:1790ŌĆō1801.   91. Atkin WS, Morson BC, Cuzick J. Long-term risk of colorectal cancer after excision of rectosigmoid adenomas. N Engl J Med 1992;326:658ŌĆō662.   92. Noshirwani KC, van Stolk RU, Rybicki LA, et al. Adenoma size and number are predictive of adenoma recurrence: implications for surveillance colonoscopy. Gastrointest Endosc 2000;51(4 Pt 1):433ŌĆō437.   94. Zhao S, Wang S, Pan P, et al. Magnitude, risk factors, and factors associated with adenoma miss rate of tandem colonoscopy: a systematic review and meta-analysis. Gastroenterology 2019;156:1661ŌĆō1674.   95. Mankaney G, Rouphael C, Burke CA. Serrated polyposis syndrome. Clin Gastroenterol Hepatol 2020;18:777ŌĆō779.   98. Tran AH, Man Ngor EW, Wu BU. Surveillance colonoscopy in elderly patients: a retrospective cohort study. JAMA Intern Med 2014;174:1675ŌĆō1682.  
|
|