External biliary drainage is required in cases where it is not possible to traverse a post-operative biliary occlusion via either endoscopic retrograde cholangiopancreatography (ERCP) or traditional interventional radiological methods. However, placement of a biliary drain in an external biliary drainage site may become dislodged, provide a source for infection, or cause dehydration and electrolyte imbalance.1 Surgical repair of iatrogenic injury can be technically difficult and may not be tolerated by patients with significant comorbidities.2,3 Sharp recanalization has been used to traverse biliary occlusions that cannot be crossed using conventional methods.4,5 Here, we present a case in which a radiofrequency (RF) wire was used to traverse an iatrogenic biliary occlusion following extended right hepatectomy for hepatocellular carcinoma.
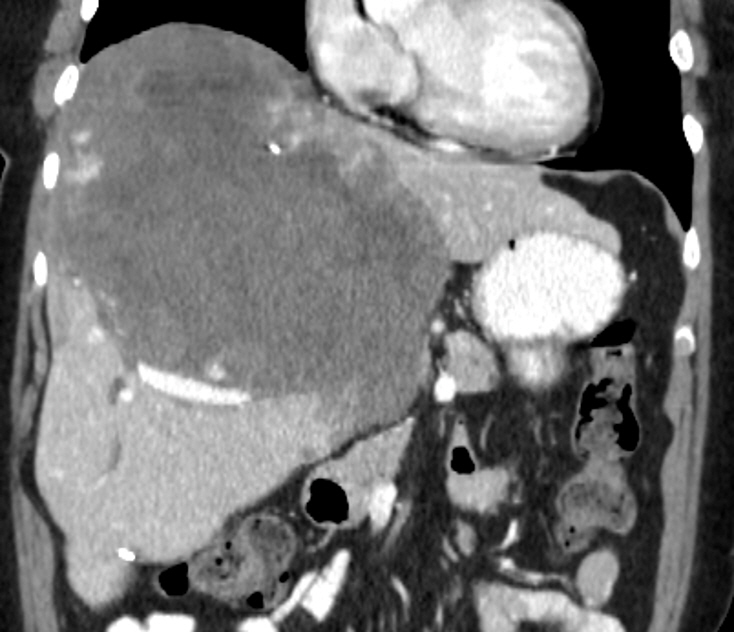
A 64-year-old woman presented 6 weeks after extensive right hepatectomy for a giant cavernous hemangioma (Fig. 1). Post-operative hemorrhage required inferior vena cava ligation and surgical Jackson Pratt drain placement in the right upper quadrant. The patient continued to have bile leakage of approximately 100 mL/24 hours. She developed significant protein-calorie malnutrition and received total parenteral nutrition as a treatment. Pertinent test results on admission included blood urea nitrogen 44 mg/dL, creatinine 1.8 mg/dL, total bilirubin 15.8 mg/dL, conjugated bilirubin 9.0 mg/dL, albumin 1.4 g/dL, alanine aminotransferase 65 IU/L, aspartate aminotransferase 84 IU/L, alkaline phosphatase 195 IU/L, white blood cell 30.1├Ś109/L, hemoglobin 7.5 g/dL, and hematocrit 22.8%.
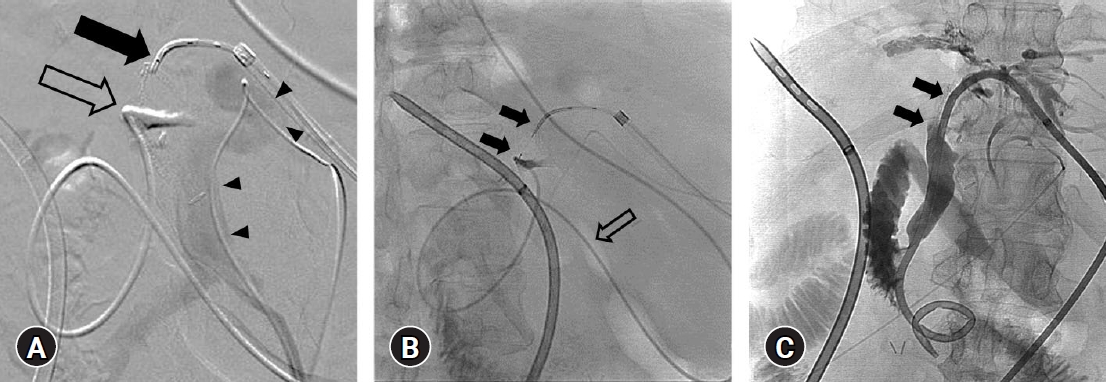
A large biloma that communicated with an isolated left biliary tree was noted upon contrast injection of the surgical drain (Fig. 2A). Percutaneous attempts to reconnect the left main bile duct to the common bile duct using a guidewire and catheters were unsuccessful. ERCP revealed non-filling of the left main bile duct (Fig. 2B). The nasobiliary drain was left in place by the endoscopist for later use by an interventional radiologist. Attempts by the radiologist to cross the occlusion using a guidewire (Fig. 2C) were unsuccessful. Tandem contrast injection of both the nasobiliary drain and the left biliary drainage catheter revealed a 2 cm distance between the left biliary tree and left main duct stump.
Pre-procedural computed tomography angiography and contrast injection of the left portal vein revealed a safe distance between the hepatic artery, portal vein, and planned trajectory across the left main duct disruption (Fig. 3A). A grounding pad (ConMed) was secured and the left biliary drainage catheter was replaced with a Cobra catheter (Cook Medical). An RF Pow┬ŁerWire (Baylis Medical) was advanced through the Cobra catheter from the left main duct across the occlusion, targeting the contrast-filled common hepatic duct, as the nasobiliary drain was retracted (Fig. 3B). The Cobra catheter was replaced with a 4-French Navicross catheter (Terumo), and the wire was replaced with an Amplatz SuperStiff guidewire (Boston Scientific). The catheter was replaced with a 10-French percutaneous biliary drain, which was placed to aid external drainage, with the distal pigtail in the duodenum (Fig. 3C). Percutaneous biliary drain drainage was 300 mL/24 hours and biloma drainage through the Jackson Pratt drain decreased to 13 mL/24 hours, with total bilirubin 11.6 mg/dL, aspartate aminotransferase 96 units/L, alanine aminotransferase 61 units/L, albumin 1.8 g/dL. There were no complications such as bleeding, bile leak, bowel perforation, or pseudoaneurysm. The patient died from anuric renal failure 19 days after the procedure.
Conventional techniques used by an endoscopist during ERCP and by an interventional radiologist during percutaneous cholangiography have limited ability to treat completely occluded biliary strictures.6 Surgical choledocho-choledochostomy is technically difficult and prohibitive in critically ill patients with existing comorbidities, and can be associated with high stricture recurrence rates.7 Restoration of bile duct continuity with either sharp recanalization or an RF wire can provide an alternative to major surgical repair of iatrogenic biliary injury, improving patient quality of life.8 However, in all cases, the visualization of a distal target is required.6
A previous study on needle cannulation described the use of a 10 mm balloon as a visual target for the needle to advance via a Cope cannula (Cook Medical) in the left biliary system.4 Another study described the use of a venous access to create a conduit from the biliary system to the jejunum with the R├Čsch-Uchida transjugular system (Cook Medical), and a sharp stylet through a curved guiding cannula under direct computed tomography imaging.5 The use of an RF wire allows surgeons to plot a controlled path towards a target.6 In this case report, we demonstrate the technically successful creation of a choledocho-choledochostomy with an RF wire after the first opacification of the target common hepatic duct through a nasobiliary drain placed by the endoscopist prior to the procedure.