Sex/gender differences in gastrointestinal endoscopy from the perspective of patients and gastroenterologists
Article information
Abstract
The sex/gender of gastroenterologists impact patients’ satisfaction, compliance, and clinical outcomes. For instance, female gastrointestinal (GI) endoscopist–patient gender concordance improves health-related outcomes. This finding suggests that it is important to increase the number of female GI endoscopists. While the number of women in the field of gastroenterology is increasing in the United States and Korea by over 28.3%, it is not enough to account for the gender preferences of female patients. GI endoscopists are at a high risk of endoscopy-related injuries. However, there is a different distribution of muscle and fat; male endoscopists are more affected in their back, while females are more affected in the upper extremities. Women are more susceptible to endoscopy-related injuries than men. There is a correlation between the number of colonoscopies performed and musculoskeletal pain. Job satisfaction is lower in young female gastroenterologists (30’ and 40’) than in the opposite gender and other ages. Thus, it is important to address these issues in the development of GI endoscopy.
INTRODUCTION
The percentage of female gastroenterologists under training has increased to 30% over 20 years in United States1 and is also increasing in Korea. As a consequence, the effect of sex/gender of gastroenterologists/endoscopists on patients’ compliance and satisfaction has been reported.2 This study suggested that female gastroenterologist–patient gender concordance improved clinical outcomes.2 That is, female patients showed a preference for female gastroenterologists, and this is consistent across the world.3-14
Most gastroendoscopic procedures are invasive and require physical strength; thus, male and female gastroenterologists face challenges in endoscopy. Sometimes, endoscopy-related injuries (ERIs) could be more serious in female gastroenterologists because of the different body structures and characteristics of endoscopic equipment. Usually, endoscopes are manufactured in one kind and they sometimes do not fit smaller hands.15 Furthermore, the muscle mass of women tends to be low16 and high levels of progesterone during pregnancy cause laxity of ligaments and joints, potentially leading to ERIs.15
Recently, the burnout problem has become important for female gastroenterologists, especially because of their domestic demands in childbearing age,17 and this issue has become more serious since February 2020, in the coronavirus disease 2019 pandemic. Doctors’ burnout problems cause negative effects not only on their own safety, but also on the viability of healthcare systems and patient care. A systemic review has suggested that intervention decreases burnout by about half and emphasized individual and structural or organizational strategies to improve the burnout problem.18 In addition, the environment around endoscopic procedures is changing likely due to surgical procedures. That is, artificial intelligence (AI) is quickly developing in various medical fields, including gastrointestinal (GI) endoscopy.19 The advent of class of deep learning method (convolutional neural network) might revolutionize the field of GI endoscopy, such as esophagogastroscopy, colonoscopy, and capsule endoscopy.19 Perhaps, this could also affect the sex/gender issue in endoscopy in the future. Based on this background, the effect of sex/gender in endoscopy was briefly reviewed from the perspective of patients and gastroenterologists.
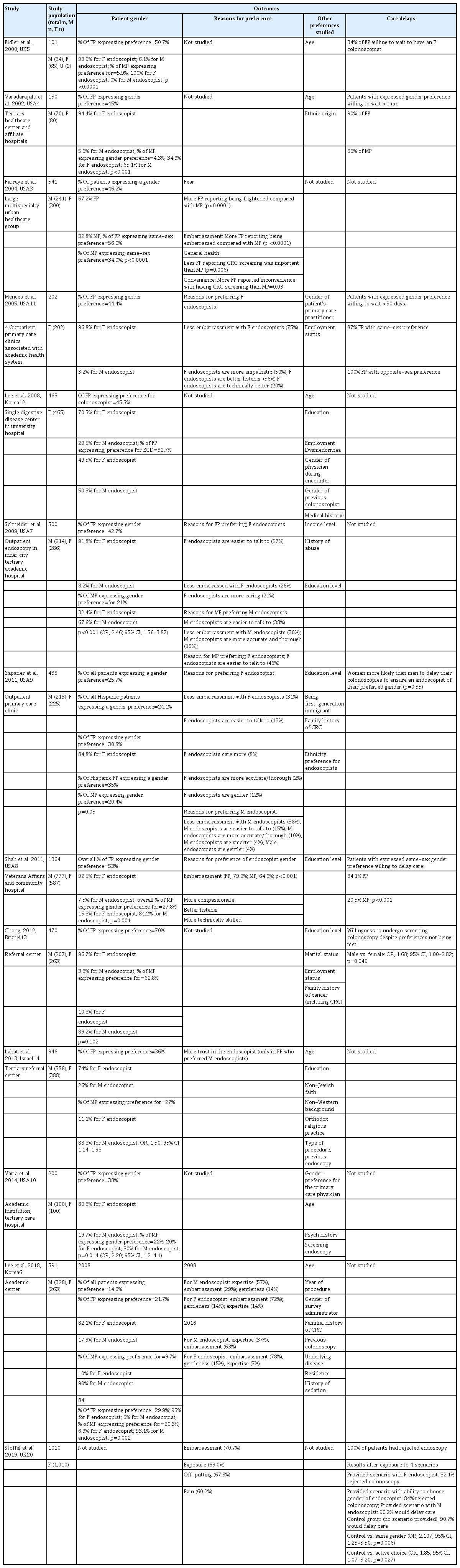
SEX/GENDER ISSUE FROM THE PERSPECTIVE OF PATIENTS
Several studies regarding patient–endoscopist sex/gender concordance have shown a meaningful gender preference for female endoscopists by female patients in the United States2 and United Kingdom.20 Endoscopists’ sex/gender can impact patients’ metrics, not only compliance, satisfaction, and follow-up, but also clinical outcomes.21,22 This is frequently found in colonoscopy, which is invasive and the fiberscope is inserted into the rectum. Female patients were found to be more likely to consider gender than male when choosing endoscopists and prefer female physicians.23,24 This situations are observed not only in the medical specialties, including gastroenterology but also surgical specialties.25,26 Gastroenterological procedures are invasive and sometimes provoke embarrassment and even fear, which become potential barriers to care.3 Seven international studies showed several key takeaways in terms of gender preference and endoscopy (Table 1).2-14,20 Among all female subjects surveyed, 22% to 70% expressed a gender preference for the endoscopists and 56% to 96.8% had a gender concordant preference.3-14 The biggest underlying reasons for the preference for female endoscopists was humiliation, especially for colonoscopy,3,7,8,11 followed by perceived characters, such as “more caring”, “gentler”, and “more compassionate”.7-9,11 Further data have been published from Western-centric countries, such as the United States and United Kingdom.2 However, comments from lesbian, gay, bisexual, transgender, and queer or questioning (LGBTQ+) individuals and individuals with disabilities have not been found in the literature so far. It is possible for these groups to have preferences for concordant gender providers. Understanding these perspectives is an important issue in medical care.2 As all the studies used locally developed surveys instead of validated questionnaire, it might be difficult to generalize the findings.2 However, there is a recent meaningful study conducted in England.27 The study re-invited previous bowel scope screening non-attenders for another appointment, and they were offered a choice of endoscopist gender.27 It was found that female non-attenders unanimously chose a female endoscopist.27 In addition, similar sex/gender preferences were found in health-seeking behaviors.2,20 A significant percentages of women chose to wait longer for an appointment with female endoscopists (34.1%–90%).4,8,9,11 However, there is a possibility that a preference for female endoscopists, could be often based on women’s characteristics, as “gentle”, “caring”, and “empathetic”.2 On the contrary, male and female patients described male endoscopists as “expertise”, “trust”, and “skillful” for their choice.6-9,11,14 Anyway there has been a report that woman provider–patient gender concordance improved clinical outcomes.28
SEX/GENDER ISSUE FROM THE PERSPECTIVE OF GASTROENTEROLOGISTS
It is well known that gastroenterologists are exposed to high risk of ERIs, which is mainly caused by continuous and repetitive use of muscles, tendons, and joints, standing for long periods, and keeping awkward positions to make difficult turns during endoscopy.15 The largest survey on ERIs (1,698 physicians)15 showed that common musculoskeletal injuries (MSIs) occurred in both genders.
The most common sites of MSIs are the thumb, neck, hand/finger, lower back, shoulder, and wrist (Fig. 1),15 which could be induced by endoscopy or hospital-related tasks, such as computer work.29 However, female endoscopists were more affected in the upper extremities whereas males in their back.29 Occupational risks related to continuous and repetitive movements contribute to MSI; however, other bias could be originated from posture-related injuries30 or chronic stress during work31 could confound the data. In any case, ERI/MSI provoked an impact on professional or ordinary activities,32 which has been confirmed by a survey of Korean gastroenterologists.17 A total of 222 gastroenterologists participated in a self-responded electronic questionnaire survey regarding daily activities and symptoms for 2 weeks.17
Surprisingly, 89.6% suffered from any grade of musculoskeletal pain, which was significantly more frequent in the female gastroenterologists (Fig. 2A).17 Female gastroenterologists showed a higher total pain score than male regardless of age group (p<0.001), especially in the age group of 30s (p<0.001, Fig. 2A).17 Regression analyses showed that sex (p<0.001), the number of colonoscopies (p=0.008) (Fig. 2B), and work-life ratio (p<0.001) were independently related to musculoskeletal pain scores.17
Musculoskeletal, gastrointestinal (GI), and mental symptoms depending on age and sex. (A) Musculoskeletal pain score. (B) Correlation between the number of colonoscopy and musculoskeletal pain. (C) GI symptoms. (D) Mental symptoms. Adapted from Jang et al. Dig Dis Sci 2020;65:86–95, with permission from Springer Nature.17
In terms of GI symptoms, 53.6% suffered from any grade of GI symptoms (Fig. 2C) and the prevalence increased with age (p=0.040).17 In addition, 68.9% had any degree of mental problems, which was more frequent in female (79.6%) than in male doctors (60.5%, p=0.002) (Fig. 2D). Women in their 30s showed the highest prevalence of any mental symptoms (87.5%, p=0.008) (Fig. 2D).17 These mental symptoms affecting normal life were related with severe musculoskeletal pain, a high number of endoscopic procedures, and a high work-life ratio independently by multivariate analysis.17 The increase of pain (p<0.001), mental symptoms (p=0.003), and GI symptoms (p=0.048) scores were correlated with increase of the work-life ratio.
The Maslach Burnout Inventory survey for the measurement of burnout showed that 64.4% met the criteria for burnout.17 That is, a high emotional exhaustion score (≥27), low personal accomplishment (≤33), and high depersonalization score (≥10) were found in 53.2%, 52.3%, and 48.7% of the respondents, respectively.17 This emotional exhaustion score was highest among women in their 30s and 40s, although it did not reach statistical significance (Fig. 3A). In addition, women in their 30s had the worst depersonalization scores (p=0.012) (Fig. 3B) and personal accomplishment domains (p=0.003) (Fig. 3C).
The job satisfaction score was lower among women (3.58±1.02) than among men (3.82±0.92, p=0.067), but without statistical significance (Fig. 4A). It was lowest among women in their 40s (p=0.049) compared with the other groups. This job satisfaction score was significantly correlated with the emotional exhaustion (p<0.001), personal accomplishment scores (p<0.001), and depersonalization (p<0.001), but not with the work-life ratio.17 Fewer female gastroenterologists answered that they would reselect to become a doctor (Fig. 4B). Furthermore, female gastroenterologists answered that they would not choose gastroenterology if they had a chance to reselect their job compared to male (Fig. 4C).17

Job satisfaction among Korean gastroenterologists and reselection job rates if they had a chance to select their job again. (A) Job satisfaction. (B) Possible reselection rate of the profession of doctor. (C) Possible reseclection rate of the profession of gastroenterologist. M, man; W, woman. Adapted from Jang et al. Dig Dis Sci 2020;65:86–95, with permission from Springer Nature.17
INTERVENTION STRATEGIES FOR THE FEMALE ENDOSCOPISTS’ BURNOUT
Due to the gender preferences of female patients, demand in the number of female gastroenterologists is increasing. This trend may continue in the future. However, the entry of women in gastroenterology fellowship programs showed that the percentage of women in the United States gastroenterology workforce is only 17.6%.33,34 This situation is more severe in other nations. For example, in the Middle East Europe, female entry into medical schools, internships, and residency programs surpassed males as in many other regions of the world,35 but this has not been directly linked to more female gastroenterologists.2 This might be related with young women’s lower job satisfaction and the gender gaps in academic societies and leadership roles.36 Thus, some effective strategies are needed in several ways as following: first, physical injuries, such as MSI, which are correlated with the number of colonoscopies, should be addressed.17 These MSIs might originate from a combination of one-size-fits-all manufacturing in spite of structural differences in our bodies.29 Marlicz et al.29 performed a systematic review of endoscopic MSIs, and they proposed a paradigm shift in the endoscopic devices and techniques in terms of comfort and safety. Recently, new computational techniques and endoscopic platforms combined with AI have been developed. Thus, we hope that this new telemedicine could help solve these technical problems in endoscopy.19,37,38 However, to prevent another similar MSI, it is also necessary to consider the sex/gender differences in the smart actuation of robotic platforms, AI-assisted endoscopy systems, and miniaturization.29
Second, to reduce burnout among young female endoscopists, diverse effective intervention trials are needed. West et al.18 performed a systemic review of intervention studies on doctor burnout. Fifteen randomized trials including 716 physicians and 37 cohort studies including 2,914 physicians met inclusion criteria from 2,617 articles.18 Intervention trials decreased overall burnout from 54% to 44% (difference 10% p<0.001; I2=15%; 14 studies) (Fig. 5), emotional exhaustion score also dropped from 23.82 points to 21.17 points (p<0.001, 40 studies), and depersonalization score from 9.05 to 8.41 (p=0.01, 36 studies), showing the efficacy of intervention trials.18 In addition, emotional exhaustion also decreased from 38% to 24% (p<0.001, 21 studies) and depersonalization from 38% to 34% (p=0.04, 16 studies).18 These suggest that various intervention trials are necessary. However, the analysis of most of these trials had not been performed based on age/sex; these evaluations need to be added. In terms of efficacy, this intervention needs to target young female endoscopists. Recently an 8-week prospective multicenter survey was conducted in Korea.39 The schedule of the intervention program was as follows: during the first 2 weeks, a questionnaire regarding daily workload and musculoskeletal symptoms was surveyed.39 Then, a novel rehabilitation program including equipment/posture correction and stretching was conducted in the following 6 weeks. Finally, follow-up daily workload and musculoskeletal symptom surveys were conducted while continuing the program for the last 2 weeks. A satisfaction survey for the program was performed at the 6th and 8th week.39 This rehabilitation program was proven helpful in improving musculoskeletal pain.39

Overall burnout. For the five randomized controlled trials and nine cohort studies reporting differences in overall burnout, the pooled mean difference estimate was a significant absolute reduction from 54% to 44% (difference, 10%; 95% confidence interval [CI], 5–14; p<0.001; I2=15%). RCT, randomized controlled therapy. Adapted from West et al. Lancet 2016;388:2272–2281, with permission from Elsevier.18
Third, further strategies are necessary to improve gender parity in the field of gastroenterology. These should include providing transparent and equitable compensation practices, encouraging fair advancement and promotion practices, and implementing protocols and processes against discrimination and harassment.40 Health systems need to support female endoscopists with policies facilitating better work-life integration, including flexibility for part-time work, job sharing, onsite childcare, and partner hiring.41 These strategies are important in the global setting, especially, where significant healthcare workforce capacity gaps are reported.2
Fourth, the higher domestic workload of female than that of male endoscopists is associated with career dissatisfaction.42 In spite of recent changes in concepts and societal trends, female endoscopists still take on more domestic responsibilities and childcare than their partners, especially during the coronavirus disease 2019 pandemic. Society and government somehow need to play an active role in the intervention of these long-lasting historical issues.
CONCLUSIONS
Recently, preference for female endoscopists by female patients has become known, and endoscopists’ sex can impact not only satisfaction and compliance, but also clinical outcomes. However, female physicians still try to avoid the field of endoscopic procedures because endoscopists perform repetitive diagnostic and therapeutic procedures with unstable postures. In fact, female endoscopists experience ERIs and are more affected in the upper extremities while men experience ERIs in their back.29 The Maslach Burnout Inventory survey, which has been performed in Korea, showed that emotional exhaustion, depersonalization, and personal accomplishment scores were worst in women in their 30s or 40s. The main reason was that female endoscopists performed more childcare and domestic responsibilities than their partners, suggesting that effective intervention is needed for young endoscopists. In addition, effective strategies are needed to improve gender parity in gastroenterology, including equitable and transparent compensation practices, fair promotion practices, and protocols and processes against discrimination and harassment. Additionally, the development of interventions (rehabilitation treatment) or new personalized devices (e.g., chair or supporting systems such as reducing the weight of endoscopy) or robot systems to reduce MSIs are necessary. Furthermore, new computational techniques and endoscopic platforms combined with AI and telemedicine could facilitate solving technical problems in endoscopies.19,38 However, it is necessary to consider sex/gender differences for the prevention of MSI in miniaturization, smart actuation of robotic platforms, and development of AI-assisted endoscopy systems, instead of handcrafted modeling.29
Notes
Conflicts of Interest
The author has no potential conflicts of interest.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (2019R1A2C2085149).