Aerosol protection using modified N95 respirator during upper gastrointestinal endoscopy: a randomized controlled trial
Article information
Abstract
Background/Aims
The coronavirus disease 2019 pandemic has affected the worldwide practice of upper gastrointestinal endoscopy. Here we designed a modified N95 respirator with a channel for endoscope insertion and evaluated its efficacy in upper gastrointestinal endoscopy.
Methods
Thirty patients scheduled for upper gastrointestinal endoscopy were randomized into the modified N95 (n=15) or control (n=15) group. The mask was placed on the patient after anesthesia administration and particles were counted every minute before (baseline) and during the procedure by a TSI AeroTrak particle counter (9306-04; TSI Inc.) and categorized by size (0.3, 0.5, 1, 3, 5, and 10 µm). Differences in particle counts between time points were recorded.
Results
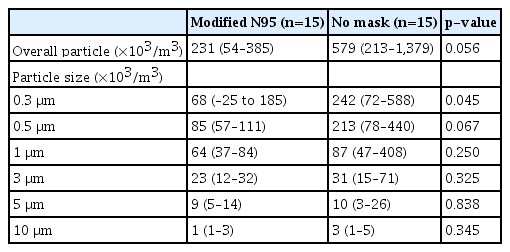
During the procedure, the modified N95 group displayed significantly smaller overall particle sizes than the control group (median [interquartile range], 231 [54–385] vs. 579 [213–1,379]×103/m3; p=0.056). However, the intervention group had a significant decrease in 0.3-µm particles (68 [–25–185] vs. 242 [72–588]×103/m3; p=0.045). No adverse events occurred in either group. The device did not cause any inconvenience to the endoscopists or patients.
Conclusions
This modified N95 respirator reduced the number of particles, especially 0.3-µm particles, generated during upper gastrointestinal endoscopy.
INTRODUCTION
Since the advent of the coronavirus disease 2019 (COVID-19) pandemic in 2019, upper gastrointestinal endoscopy has been considered an aerosol-generating procedure.1-3 Several studies have demonstrated the presence of the causative sudden acute respiratory syndrome coronavirus-2 virus in body fluids such as in oropharyngeal secretions. The viral infection is known to spread by aerosol particles <5 µm and droplets >5 µm in size.4-6 Endoscopic procedures have been adjusted to prevent human-to-human transmission.7 For treating patients with COVID-19, full personal protective equipment is mandatory for endoscopists and other healthcare personnel.8,9 However, some patients who test negative for COVID-19 before endoscopy may develop viral infection during the incubation period. Therefore, adequate protection of endoscopy personnel is required to prevent viral spread.
Various novel devices were developed to prevent viral dissemination during endoscopic procedures.10-15 An acrylic box was adapted for endotracheal intubation in COVID-19 patients to decrease the spillage of aerosols and droplets.16 The N95 respirator is a well-known and widely available mask that can filter at least 95% of 0.3-µm particles. Although COVID-19 viral particles are 0.125 µm in diameter, they are mostly adherent to body fluids. Since the N95 respirator can filter aerosols and droplets, thereby preventing viral transmission,17 here we modified the mask to enable endoscopic insertion and measured its efficacy for particle release during upper gastrointestinal endoscopy. We then assessed patient safety and endoscopist feedback.
METHODS
Study design
This study was conducted at the Siriraj Gastrointestinal Endoscopy Center (World Gastroenterology Organization–accredited training center), Faculty of Medicine, Siriraj Hospital, Mahidol University, Thailand.
Design of modified N95 respirator
A standard N95 respirator (3 M Aura 1870+ model; 3M Health Care) was modified to create a channel for endoscopic insertion. In proportion to the 9.9-mm outer diameter of the gastroscope (GIF-HQ190; Olympus), two intersecting 10.4-mm linear puncture holes were created to fit the diameter of the scope to minimize aerosol spread during the procedure. A representative illustration of the modified N95 respirator is provided in Figure 1.

Illustration of modified N95 respirator. A standard N95 respirator (3M Aura 1870+ model) was modified as shown. In proportion to the 9.9-mm outer diameter of the gastroscope (GIF-HQ190; Olympus), two intersecting 10.4-mm linear holes were created and fitted to the diameter of the scope. Illustrated by the author.
Participants
All patients aged ≤18 years with undetectable COVID-19 on a nasopharyngeal swab tested by reverse transcriptase polymerase chain reaction within 48 h of diagnostic upper gastrointestinal endoscopy were enrolled. Patients who required orotracheal intubation, required a transnasal endoscopy route, or had a previous history of upper gastrointestinal surgeries and unrelated procedures were excluded. All eligible patients were monitored during the procedure by an anesthesiologist.
Randomization and procedure
The participants were randomly assigned in a 1:1 ratio to the modified N95 or control group (no mask) using a computer-generated randomization program. Group allocation was performed by a nurse not involved in the procedure using sealed opaque envelopes. After allocation, each patient was transferred to the endoscopic unit and the endoscopic room was sealed to avoid unnecessary traffic that could interfere with particle counts during the procedure. Due to the nature of the intervention, the endoscopists and patients could not be blinded. All procedures were performed in one of two endoscopic rooms: A, room volume of 90 m3 with an air flow change of 25 times/h, and B, room volume of 135 m3 with an air flow change of 15 times/h. The endoscopists and other involved personnel wore surgical masks, gowns, disposable latex gloves, and closed-toe shoes or shoe covers throughout the procedure. All patients were placed in the left lateral decubitus position using supplemental oxygen via a nasal cannula. Anesthesia was chosen based on the anesthesiologist and patient’s joint approval. For topical anesthesia before endoscopy, five puffs of 10% lidocaine were sprayed in the patient’s mouth twice and retained for 10 seconds each time. A negative gag reflex was confirmed before the endoscopy commenced. For intravenous sedation, 25 to 75 µg/kg/min of propofol and 1 µg/kg of fentanyl were injected intravenously to achieve mild to moderate sedation as per the definition given in the American Society of Anesthesiologists guideline.18 After adequate anesthesia and oxygenation were ensured, a modified N95 respirator was placed over the patient’s nose and mouth in the modified N95 group and an endoscope inserted through the channel. Endoscopic examinations were performed in both groups.
Outcome measurements
A TSI AeroTrak (9306-04) handheld particle counter (TSI Inc.) was used to determine the total number of particles (Fig. 2). The counter has an acquisition flow rate of 2.83 L/min. Recorded particle sizes were 0.3, 0.5, 1, 3, 5, and 10 µm. The particle counter was placed 1 m away from the patient. The setup of the endoscopic unit is shown in Figure 3. Baseline particle counts were measured in the empty endoscopic room with closed doors for at least 15 minutes in the early morning before the first case of endoscopy that day. During each endoscopic examination, particle counts were measured and recorded every minute from the time of scope intubation to complete scope withdrawal. The primary outcome was the intergroup difference in particle counts during the procedures. The secondary outcomes were factors associated with increased particle counts and adverse events in patients wearing the modified N95 respirator. Feedback from patients and endoscopists was collected after every procedure. Patient demographic data, anesthetic techniques, and details of the upper gastrointestinal endoscopy were recorded.
Statistical analysis
Statistical analysis was performed using SPSS software ver. 18.0 (SPSS Inc.). Continuous variables are expressed as number (%) and mean±standard deviation for normally distributed variables and median with interquartile range (IQR) for non-normally distributed variables. The increased intergroup particle counts were compared using the Mann-Whitney U-test. Factors associated with changes in particle counts during the procedure were analyzed using bivariate correlations. Values of p<0.05 were considered statistically significant.
Ethical statements
This single-center randomized controlled study was approved by the Siriraj Institutional Review Board (approval number: Si-017/2022) and registered in the Thai Clinical Trials Registry (TCTR20220121006). Written informed consent was obtained from all participants.
RESULTS
Demographic data
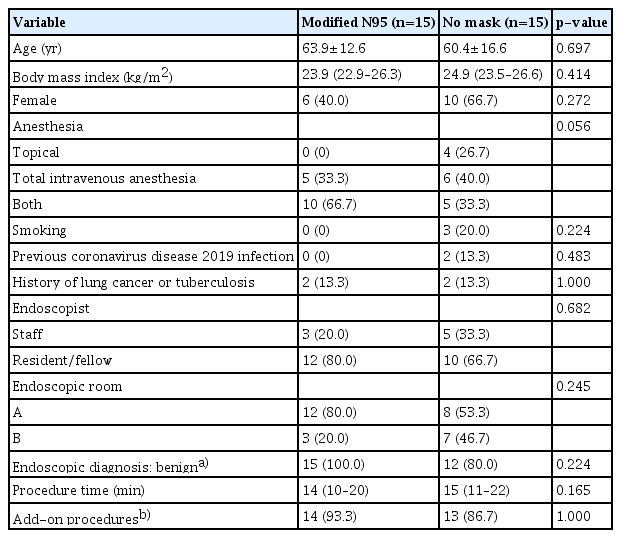
The demographic data and endoscopic details of the N95 and control groups were comparable, including the nature of the disease and procedure time (Table 1). The baseline total particle counts of all particle sizes were also comparable between groups (358; IQR, 276–689 vs. 399; IQR, 288–753×103/m3; p=0.279).
Increased particle counts during endoscopic procedure
A statistically significant increase in 0.3 micron particle size was observed in the control group (242 vs. 68×103 counts/m3; p=0.045). The concentration of 0.3-µm particles was higher, but not statistically significant, in the control group. The control group had greater than two times the overall particles of the modified N95 group (Table 2).
Factors affecting increased particle counts
Our study found no correlation between the following factors: body mass index, choice of anesthesia, smoking, previous history of COVID-19 infection or respiratory tract disease, endoscopic duration, and overall increased particle count in either group (Table 3).
Adverse events
No complications were observed during or after the endoscopic examination in this study. Specifically, respiratory compromise or secretion obstruction were not observed in the modified N95 group during endoscope insertion. In addition, the endoscopists reported an absence of difficulty with endoscope insertion in the modified N95 group. All patients underwent one successful endoscope insertion attempt through the channel created in the modified N95 respirator.
DISCUSSION
Our study assessed the advantages and safety of using a modified N95 respirator for controlling aerosol dissemination in patients that undergo upper gastrointestinal endoscopy. The study demonstrated that our modified N95 respirator reduced overall particle spillage by approximately 50% and significantly decreased 0.3 micron particle spillage by 72% versus patients who were unmasked during the endoscopic examination. This suggests that the transmission of COVID-19 viral particles that adhere to aerosols from body fluids can be prevented. Additionally, the respirator did not interfere with endoscopic examination or increase patient complications.
In the recent years of the COVID-19 pandemic, several innovations were proposed for aerosol and droplet prevention.10-15 A transparent acrylic box placed over the patient’s head effectively reduced the spillage of droplets but interfered with the work of endoscopists.19 In addition, dental suction reduces the number of particles of all sizes that were detected during upper gastrointestinal endoscopy.20,21
Topical anesthetic throat spray and coughing were strongly associated with maximal particle generation throughout upper gastrointestinal endoscopic procedures.22,23 In our study, we did not apply any suction devices, as this was not feasible in patients with masks. However, reflex coughing is blunted by intravenous sedation, as seen in patients of our study. It would be interesting to examine the beneficial effects of our respirator in patients undergoing upper gastrointestinal endoscopy without sedation.
Owing to the insignificant intergroup difference in counts of particles >0.3 µm, it is possible that the movement and activities of endoscopists and other healthcare personnel in the procedure room could have generated additional particle counts. The additional procedure, rapid urease test or biopsy, requires an additional instrument that is normally kept in a sealed package to avoid diffusion of dust into the air due to its unsealing. Moreover, larger particles can attach to droplets trapped within the mask or gravitate toward the ground before reaching the particle counter. In this study, the particle counter was kept 1 m apart from the patient’s mouth as the distance between the patient’s mouth and the endoscopist’s nose was estimated to be approximately 1 m. Further, a shorter distance could have interfered with the endoscopic procedure.24
The strength of this randomized study was the presence of a controlled environment (only two endoscopic rooms with limited traffic were used). Both staff and trainee endoscopists reported no difficulty during endoscopy in patients wearing masks, indicating that a modified N95 respirator could be effectively applied in daily practice. The original N95 respirator is widely available and the N95 respirator modification technique is simple, replicable at any hospital. The application of this modified N95 respirator is protective and practical for patients who may carry the risk of COVID-19 infection and present during their incubation period.
This single-center randomized study has some limitations. First, it included only uncomplicated upper gastrointestinal endoscopies. Therefore, the beneficial effect of respirators on particle reduction in advanced endoscopic interventions such as endoscopic retrograde cholangiopancreatography or endoscopic submucosal dissection should be established. Prolonged endoscopic duration, when multiple additional instruments are inserted through the working channel of the scope, may affect the capability of the mask. Second, the particle counter used to detect particle at 1 m in this study was limited to the detection of 0.3-µm particles. Different particle counters at variable distances may yield differing results. Finally, we used particle size as a surrogate marker for possible airborne viral spread. Whether particle reduction decreases the rate of airborne infection needs to be examined.
In conclusion, this study demonstrated that a modified N95 respirator could reduce the counts of the smallest (i.e., 0.3-µm) particles and decrease the counts of larger particles. Therefore, we conclude that the modified N95 respirator can be safely applied in patients requiring upper gastrointestinal endoscopy, without increasing procedural difficulty for the endoscopist.
Notes
Conflicts of Interest
The authors have no potential conflicts of interest.
Funding
None.
Acknowledgments
We thank Mr. Asadavudh Buachum and Miss Kanyanat Changpan from the Occupational Health Division for their cooperation with the particle measurements and Dr. Saowalak Hunnangkul for her assistance with the statistical analysis.
Author Contributions
Conceptualization: CN, TA; Data curation: CN, TA, TT; Formal analysis: CN, TA; Investigation: CN, TA, AM, TS; Methodology: CN, TA, VC; Project administration: CN, TA, JS, TP, TT; Resources: CN; Supervision: TA, VC, AM, VL; Validation: CN, TA, VL; Visualization: JS, AT, CP, TP, VT, NS; Writing–original draft: CN; Writing–review & editing: all authors.