Prevalence, natural progression, and clinical practices of upper gastrointestinal subepithelial lesions in Korea: a multicenter study
Article information
Abstract
Background/Aims:
This study aimed to evaluate the prevalence and natural progression of subepithelial lesions (SELs) in the upper gastrointestinal (UGI) tract.
Methods:
The medical records of patients with UGI SELs who underwent endoscopic screening at eight university hospitals between January and December 2010 were retrospectively investigated. The follow-up evaluations were performed until December 2016.
Results:
UGI SELs were found in 1,044 of the 65,233 participants screened (endoscopic prevalence, 1.60%; the total number of lesions, 1,062; mean age, 55.1±11.2 years; men, 53.6%). The median follow-up period was 48 (range, 8–74) months. SELs were most frequently found in the stomach (63.8%) and had a mean size of 9.9±6.1 mm. Endoscopic ultrasonography (EUS) was performed in 293 patients (28.1%). The most common lesions were leiomyomas, followed by gastrointestinal stromal tumors (GISTs), and ectopic pancreas. The proportions of SELs with malignant potential according to size were 3% (<1 cm), 22% (1–2 cm), 27% (2–3 cm), and 38% (≥3 cm). In gastric SELs larger than 1 cm, resections were performed in 20 patients because of an increase in size, of which 12 were found to be GISTs.
Conclusions:
The prevalence of UGI SELs was 1.60%. Further, 23% of gastric SELs ≥1 cm were precancerous lesions, most followed by EUS and clinical decisions without initial pathological confirmation.
INTRODUCTION
Subepithelial lesions (SELs) in the gastrointestinal (GI) tract include lesions with a smooth prominence in the inner cavity of the GI tract and no changes in the mucosal surface on endoscopy. SELs are subepithelial tumors in the GI wall layer that grow under the epithelium. SELs are typically classified as non-neoplastic or neoplastic. Most lesions are asymptomatic and clinically insignificant. However, neuroendocrine tumors (NETs), lymphomas, glomus tumors, and gastrointestinal stromal tumors (GISTs) are often malignant or potentially malignant. Despite state-of-the-art endoscopic facilities and extensive research, SELs are still difficult to diagnose before surgery using noninvasive methods, such as endoscopy or endoscopic ultrasound (EUS). Histological diagnosis of lesions includes bite-on-bite biopsy, EUS-guided fine needle aspiration/biopsy (FNA/B), endoscopic mucosal resection/endoscopic submucosal dissection, and submucosal tunneling with endoscopic resection.1-3 To detect and treat malignant lesions early, appropriate diagnostic approaches are required according to the characteristics of the lesions.4,5
Globally, there are few reports on the prevalence of upper GI SELs. Endoscopic identification has increased in recent years owing to the development of endoscopic technologies and increased interest in upper GI SELs.6 In Korea, the incidence of upper GI SELs from a single-center study was reported to be 0.8% to 1.7%, but these data are insufficient; there are no established guidelines, and hence each hospital uses a variety of approaches.7,8
The current clinical guidelines suggest that hypoechoic lesions in the second or third layers are removed if they are symptomatic or larger than 2 cm; even in the absence of symptoms, as much of the pathology is obtained as possible.9 On the other hand, SELs on the fourth layer are recommended for removal unconditionally due to the possibility of GISTs.4 EUS images often cannot distinguish malignant lesions and third-layer tumors. In Korea, esophagogastroduodenoscopy (EGD) is frequently performed, and endoscopic resections have also been developed.10-12 Therefore, it is necessary to assess whether the guidelines are followed in actual clinical conditions. We investigated the incidence, clinical practice patterns (diagnostic approaches), and the natural progression of upper GI SELs.
METHODS
Subjects
This multicenter retrospective study was conducted between 2010 and 2016 at the EUS Research Group of the Korean Gastrointestinal Endoscopy Society. The medical records of patients with upper GI SELs among the population who underwent endoscopic screening at eight university hospitals between January 1 and December 31, 2010, were retrospectively analyzed. These participants, in whom SELs were found, were followed up for 6 years through to 2016. Gastroscopy and EUS reports and clinical courses were reviewed.
Definitions
Diagnoses were divided into clinical and pathological. Pathological diagnoses were made using endoscopic biopsy, EUS-guided FNA/B, endoscopic resection, or surgical resection. If a pathological diagnosis could not be obtained, a clinical diagnosis was made by tracking the clinical progress for more than 1 year and ultrasound imaging.
Examinations and endpoints
First, for each healthcare center, the number of patients with SELs found during gastroscopy was checked in those who had undergone endoscopy for 1 year, and the number of patients who received additional tests, such as EUS, computed tomography, and biopsy. In addition, the percentage of patients who underwent endoscopic or surgical resection was determined, and those who did not undergo resection were followed up until 2016. During follow-up, the number and interval of follow-ups, size change of the SEL, and presence or absence of tumor resection were identified.
The primary endpoint was the incidence of upper GI SELs in asymptomatic patients. The secondary endpoints were clinical practice patterns and natural courses.
Ethical statements
The Institutional Review Board of each hospital approved the study protocol (KC20RIDI0036).
RESULTS
Prevalence and characteristics of upper GI SELs
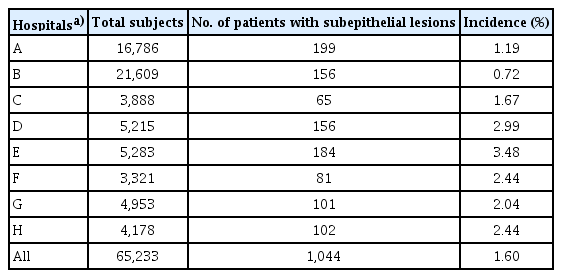
Between January 1 and December 31, 2010, 65,233 individuals underwent screening endoscopies at eight university hospitals. Upper GI SELs were identified in 1,044 patients (1,062 lesions in total). Thus, the endoscopic prevalence of upper GI SELs was thus 1.60%. The prevalence differed significantly between institutions (range, 0.72%‒3.48%; Table 1). The median age of the participants was 56 years (range, 12‒86 years, mean 55.1±11.2 years), and 560 participants (53.6%) were men. Eighteen patients (1.7%) had two or more tumors. If an external indentation or vascular structure could be distinguished by endoscopy or other imaging studies, it was excluded from the SELs.
The most common location was the upper third of the stomach (39.9%). Ten of the 14 histologically confirmed GISTs were located in the upper body. The mean size of the SELs when they were first identified on endoscopy was 9.9±6.1 mm, and 49.1% of the SELs were 1 cm or larger, 7.0% were larger than 2 cm, and 1.7% were larger than 3 cm (Table 2).
Among the 1,044 patients with SELs identified by EGD, 293 (28.1%) underwent additional endoscopic ultrasonography. The EUS characteristics of the upper GI SELs according to the organ are described in Table 3. A total of 154 lesions (14.8%) were biopsied. The histological results of the biopsy confirmed were as follows; esophageal duplication cyst (1), esophageal or gastric leiomyoma (11), esophageal hemangioma (1), gastric or duodenal ectopic pancreas (10), gastritis cystica profunda (1), inflammatory fibrinoid polyp (1), lipoma (1), gastric adenocarcinoma (1), Brunner’s gland hyperplasia (7), duodenal lymphangioma (2), and duodenal neuroendocrine tumor (1).
A total of 394 SELs were followed up for >12 months, with a median of 54 months (range, 12‒83 months); of these, the esophagus, stomach, and duodenum SELs were followed up 59 (range, 12–77) months, 52 (range, 12‒83) months, and 60 (range, 12‒82) months, respectively. Fifty-four patients (5.2%) had their SELs removed by endoscopic procedures or surgery, 29 immediately after diagnosis, and 25 during follow-up, owing to increased SEL sizes (Fig. 1). The final histological results of the 54 resected SELs were as follows: GIST (11); leiomyoma (10); ectopic pancreas (10); NET (3); granular cell tumor (3); Brunner's gland adenoma (3); lipoma (2); inflammatory fibroid polyp (2); schwannoma (1); advanced gastric cancer (1); lymphoepithelioma-like carcinoma (medullary carcinoma) (1); eosinophilic abscess (1); ectopic gastric mucosa (1); and not mentioned (5)
Types and distribution of SELs according to the location
The most common SELs among all the upper GI SELs were leiomyomas (30.4%), followed by GISTs (24.6%), ectopic pancreas (16.7%), and lipomas (5.1%) (Table 4). The most common SELs in the stomach were GIST (39.1%), ectopic pancreas (22.5%), and leiomyoma (18.3%). Common SELs in the esophagus were leiomyoma (75.8%) and granular cell tumor (15.2%), whereas common SELs in the duodenum were Brunner's gland hyperplasia/adenoma (29.3%) and lymphangioma (22.0%).
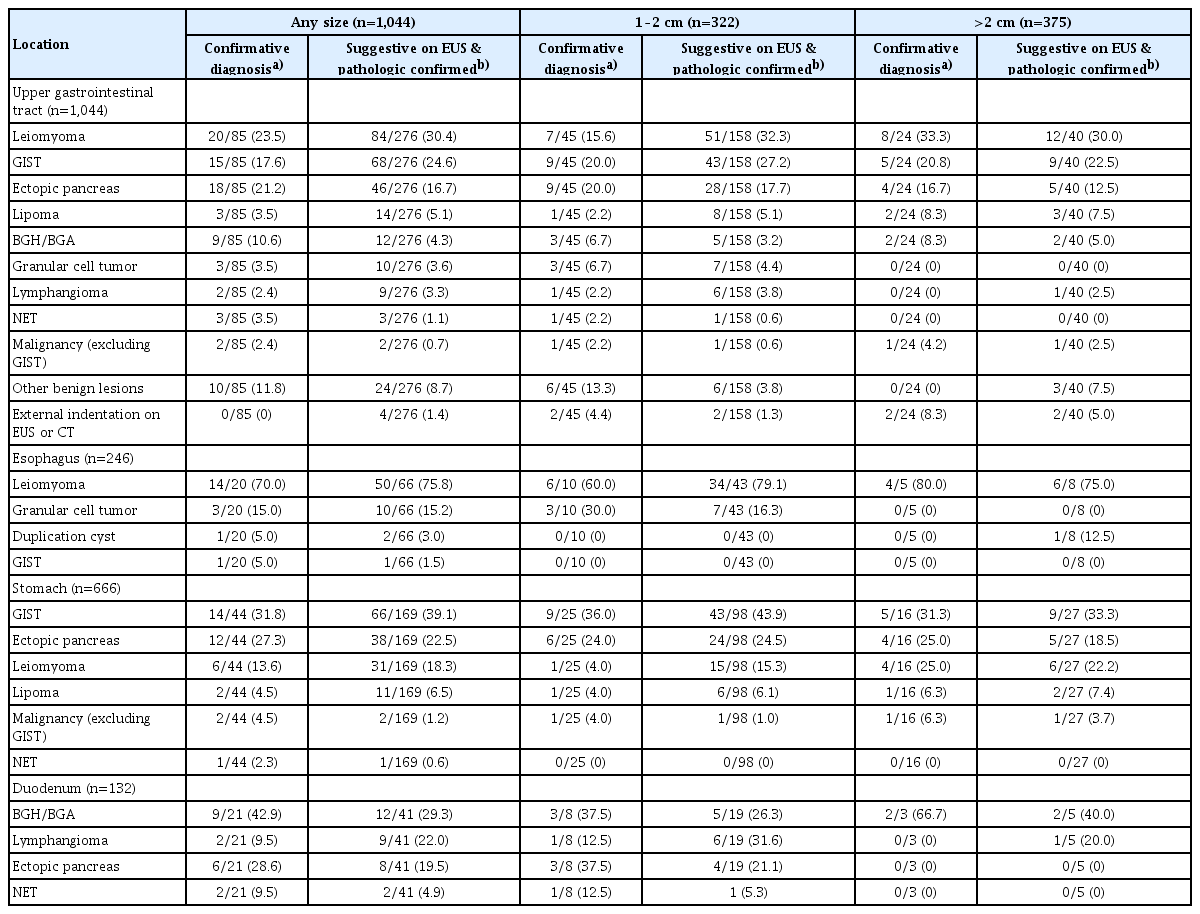
The frequency order of the subepithelial lesions according to the location of the upper gastrointestinal tract
Some SELs were uniquely distributed in the esophagus and duodenum. For example, granular cell tumors (15% of esophageal SELs) occur in the esophagus. Brunner's gland hyperplasia/adenoma (29% of duodenal SELs) and lymphangiomas (22% of duodenal SELs) were observed in the duodenum.
Forty-four esophageal and gastric SELs were greater than 2 cm in size. Among them, the proportion of malignant SELs was 18% (seven GISTs and one adenocarcinoma; Fig. 2). In the stomach, the proportion of malignant SELs increased with size, with 3% of SELs >1 cm, 29% of SELs >2 cm, and 38% of SELs >3 cm.
Distribution of upper gastrointestinal subepithelial lesions (SELs) according to size. (A) Types of SELs of 2 cm or more. (B, C) Comparison of the proportion of malignancy or premalignant gastric SELs by size. Malignancy or premalignant lesions included gastrointestinal stromal tumors, neuroendocrine tumors, and gastric cancer. BGH, Brunner’s gland hyperplasia; Ext., external; GIST, gastrointestinal stromal tumor.
Natural course of upper GI SELs
Figure 3 shows the clinical practice patterns of gastric SELs greater than 1 cm and gastric SELs greater than 2 cm. Further, 34 stomach SELs measured >2 cm in size. Eight SELs were pathologically diagnosed, and 3 SELs proved to be malignant (one adenocarcinoma and two GISTs). Additionally, 22 SELs were followed up without pathological confirmation (median, 48 months; range, 8–74 months). Seven gastric SELs >2 cm increased in size during a median follow-up period of 60 months (range, 45 to 74 months) and were resected endoscopically or surgically. Fifteen SELs remained unchanged in size or shape during the median follow-up period of 46 months (range, 8–61 months). Eventually, 65% of gastric SELs >2 cm were clinically followed up without a pathological diagnosis; among them, 13.6% (3/22) were found to be malignant.
Natural course of gastric subepithelial lesions (SELs) according to size. (A) Gastric SELs measuring 1 to 2 cm in size. (B) Gastric SELs larger than >2 cm. Bx., biopsy; GCP, gastritis cystica profunda; IFP, inflammatory fibroid polyp; FNA/B, fine needle aspiration/biopsy; ER, endoscopic resection; Eo., eosinophilic; GIST, gastrointestinal stromal tumor; AGC, advanced gastric cancer.
Figure 4A shows the practice patterns of the 246 esophageal SELs. The pathological analysis confirmed leiomyomas in 17 patients. A total of 105 (42.7%) patients were followed up without pathological confirmation. Four patients underwent SEL resection because of an increase in size.
Clinical practice and natural course of (A) esophageal and (B) duodenal subepithelial lesions. Bx., biopsy; ER, endoscopic resection; GCT, granular cell tumor; GIST, gastrointestinal stromal tumor; F/U, follow-up; BGA, Brunner’s gland adenoma; BGH, Brunner’s gland hyperplasia; NET, neuroendocrine tumor; FNA, fine needle aspiration.
Approximately 37 of the 132 patients with duodenal SELs attempted to obtain a pathological diagnosis (Fig. 4B). Twenty patients were pathologically confirmed at their first detection, and two were diagnosed with endoscopic resection of an NET. Among those with confirmed duodenal SEL, 33 (25.0%) were followed up without a pathological diagnosis. Four SELs that had increased in size during the follow-up period were resected. The malignant potential was observed in 1.5% (2/132) of duodenal SELs (duodenal NETs).
A total of 35 SELs (seven esophageal, 24 gastric, and four duodenum SELs) increased in size during the median 58 months follow-up period (range, 12–73 months; mean, 51.5±17.5 months). The size of SELs was 1.3±0.4 cm at the initial diagnosis and 2.0±0.8 cm at the last follow-up or excision. The pathologies were GIST in five patients, leiomyoma in three patients, ectopic pancreas in one patient, and others that could not be identified.
DISCUSSION
This study evaluated the prevalence and natural progression of upper GI SELs detected during endoscopic screening. We also evaluated the clinical practice patterns of upper GI SELs. The prevalence in the total screening population was 1.6% (1,044 out of 65,233). The institutional prevalence varied from 0.72% to 3.48%. In previous studies, the prevalence of upper GI SELs in the screening population was 0.8% to 1.7%.7,8 Studies performed in the Korean population were 0.8% to 1.1% during 2010–2022. These large differences between institutions suggest that the detection of upper GI SELs may depend more on the fidelity of the endoscopist or endoscopic records than on an increase in the actual prevalence or development of endoscopic techniques.
In this study, 54 SELs were endoscopically or surgically resected immediately after diagnosis, and 28 SELs were resected during follow-up owing to their increased size. Considering that the SELs lost during follow-up were not counted, there is likely to be an increase in tumor size. Several studies investigated the natural history of upper GI SELs. Lim et al.7 reported an increase in the size of SELs in only 8 (3.2%) of 252 SELs over 84 months.Other studies showed that only 8.5% of 989 SELs changed significantly in size and morphology at a median follow-up period of 24 months (range, 3–123 months).
Most SELs are benign at diagnosis. NETs, lymphomas, glomus tumors, and GISTs are generally malignant or likely to become malignant. Endoscopy makes it difficult to predict malignant tumors based solely on the tumor shape. A possible diagnosis can be made by synthesizing endoscopic characteristics, such as tumor location, organ, mobility, and consistency.13 In general, additional diagnostic modalities of EUS are required. In this study, only 28.1% (293/1,044) of the SELs underwent additional EUS. This may have included some SELs already discovered before the study and those undergoing follow-up. The common frequency of tumors by organ was not significantly different from that reported in previous studies. GISTs are the most common SELs of the stomach.
Small, incidentally detected SELs can be monitored periodically using endoscopy or EUS. The European Society of Gastrointestinal Endoscopy guidelines recommend that the management of each SEL depends on its size, location, pathology, and malignant potential or symptoms.14,15 A pathological diagnosis is recommended if the lesion is larger than 2 cm or if EUS suggests malignancy.16 Several SELs, such as lipomas, cysts, or ectopic pancreas, show typical characteristics during endoscopy or EUS. However, the diagnostic accuracy of EUS for SELs located in the third and fourth layer is unsatisfactory without pathology. Tissue acquisition for histopathological diagnosis is often necessary to decide further treatment policies.17-19 SELs arising from the submucosa and muscularis propria can be sampled using tunnel biopsies (or deep-well biopsies), EUS-guided FNA/B, or advanced endoscopic techniques (unroofing or endoscopic resection).2,20-25
This study has some limitations. First, the prevalence rates varied among different institutions, suggesting that the incidence may depend on the endoscopist. Second, because this was a retrospective study, it was impossible to review all endoscopic images. Pathological diagnosis, which is the gold standard, was not performed for all lesions; therefore, it was impossible to calculate an accurate diagnosis.
In this study, the tissue yield for the pathological diagnosis of upper GI SEL was not high at approximately 44%. Therefore, it is important to follow up according to clinical judgment using endoscopy and EUS findings, as well as a biopsy. In this study, in the stomach, the proportion of malignant SELs increased as the size increased, and in the case of upper GI SELs of size 1 cm or larger, it is necessary to recommend additional tests, such as biopsy or EUS. If the pathology cannot be confirmed, close follow-up may be needed.
In conclusion, the prevalence of SELs in the upper GI tract was 1.60% in an endoscopically screened population. In the case of the stomach, where GIST occurs, it is necessary to recommend additional tests such as biopsy or EUS if the size is ≥1 cm
Notes
Conflicts of Interest
Gwnag Ha Kim is currently serving as a deputy editor in Clinical Endoscopy; however, he was not involved in the peer reviewer selection, evaluation, or decision process for this article. The authors have no potential conflicts of interest.
Funding
None.
Author Contributions
Conceptualization: GHK; Data curation: YC, YKC, GHK, JHC, ESK, JHK, EKC, THK, SHK; Formal analysis: YC, YKC; Supervision: YKC, GHK; Software: YC; Project administration: GHK, JHC, JHK; Writing–original draft: YC; Writing–review & editing: all authors.