Management of Non-Variceal Upper Gastrointestinal Bleeding
Article information
Abstract
Upper gastrointestinal bleeding (UGIB) is a critical condition that demands a quick and effective medical management. Non-variceal UGIB, especially peptic ulcer bleeding is the most significant cause. Appropriate assessment and treatment have a major influence on the prognosis of patients with UGIB. Initial fluids resuscitation and/or transfusion of red blood cells are necessary in patients with clinical evidence of intravascular volume depletion. Endoscopy is essential for diagnosis and treatment of UGIB, and should be provided within 24 hours after presentation of UGIB. Pre-endoscopic use of intravenous proton pump inhibitor (PPI) can downstage endoscopic signs of hemorrhage. Post-endoscopic use of high-dose intravenous PPI can reduce the risk of rebleeding and further interventions such as repeated endoscopy and surgery. Eradication of Helicobacter pylori and withdrawal of non-steroidal anti-inflammatory drugs are recommended to prevent recurrent bleeding.
INTRODUCTION
Non-variceal upper gastrointestinal bleeding (UGIB) is a critical clinical condition that requires an urgent management. Although there was a significant reduction in the incidence of bleeding peptic ulcers with the introduction of proton pump inhibitor (PPI) and eradication of Helicobacter pylori,1,2 UGIB still remains a clinically important issue due to the increase in the proportion of elderly population, use of non-steroidal anti-inflammatory drugs (NSAIDs) and in-hospital UGIB. This review focuses on recently published articles addressing the management of acute non-variceal UGIB.3-5
INITIAL ASSESSMENT AND RISK STRATIFICATION
The first step in the management of patients presenting with overt UGIB is the assessment of hemodynamic status and initiation of resuscitative measures as needed. Intravenous (IV) fluids and transfusion of red blood cells targeting hemoglobin level of ≥7 g/dL may be required in euvolemic patients. Higher hemoglobin levels may need to be targeted in patients with clinical evidence of intravascular volume depletion or comorbidities such as coronary artery disease.
Risk assessment of patients is clinically useful to determine which patients are at higher risk of further bleeding and may aid in making management decisions such as timing of endoscopy, time of discharge and level of care. The widely studied methods used to assess risk and to predict risk of rebleeding and mortality include the Rockall score6 and Blatchford score.7 In a recent study from Hong Kong,8 patients who needed endoscopic treatment showed a significantly higher Blatchford score and a threshold of more than 1 (high risk) was useful for predicting patients who needed endoscopic treatment; however, Rockall score could not definitely identify higher risk patients in this study. On the other hand, another study from United Kingdom showed that patients who were classified as low risk with Blatchford score of 0 and were managed on the outpatient bases showed no additional adverse events, and that the proportion of admitted patients also fell.9
PRE-ENDOSCOPIC CARE
Recent consensus suggests that nasogastric or orogastric lavage is not helpful in patients with UGIB for diagnosis, prognosis, visualization, or therapeutic effect.3,5
A Cochrane meta-analysis of six randomized trials of pre-endoscopic PPI therapy found no significant differences between PPI group and control in mortality (odds ratio [OR], 95% confidence interval [CI] 1.12, 0.72 to 1.73), rebleeding (OR, 95% CI, 0.81, 0.61 to 1.09), or surgery (OR, 95% CI, 0.96, 0.68 to 1.35). However, pre-endoscopic use of PPIs significantly reduced the proportion of patients with high-risk stigmata (OR, 95% CI, 0.67, 0.54 to 0.84) and the need for endoscopic therapy (OR, 95% CI, 0.68, 0.50 to 0.93) compared with patients who received placebo or a histamine-2 receptor antagonist.10 A large single-center randomized controlled study also showed the benefit of pre-endoscopic high-dose IV PPI therapy in downgrading the stigmata of hemorrhage at index endoscopy.11
TIMING OF ENDOSCOPY
Observational studies showed the benefit of endoscopy within 24 hours after admission in terms of decreasing length of stay and surgical intervention.12,13 Therefore, it is recommended that all hospitals provide sufficient resources for an endoscopy service that can offer an examination within 24 hours after patient presentation, including weekends and holidays. In addition, in very high risk patients who are hemodynamically unstable and those who present with massive hematemesis, endoscopy should be performed as soon as they are stabilized through resuscitation.14
ENDOSCOPIC THERAPY
Endoscopic therapy is considered according to the stigmata of recent hemorrhage which indicates the appearance of an ulcer base at endoscopy in patients with ulcer bleeding. The stigmata can predict the risk of further bleeding and the need for therapeutic intervention.15,16 The Forrest classification is commonly used to describe the stigmata in Europe and Asia. In this classification, grade I represents active hemorrhage, grade II denotes recent stigmata of bleeding, and grade III indicates no stigmata of recent hemorrhage (Fig. 1).15,17 Endoscopic therapy should be provided to patients with active spurting or oozing of blood or a non-bleeding visible vessel. The role of endoscopic therapy for ulcers with adherent clot is controversial.18 However, endoscopic therapy may be considered in patients with adherent clot resistant to vigorous irrigation, especially for those with higher risk of rebleeding.
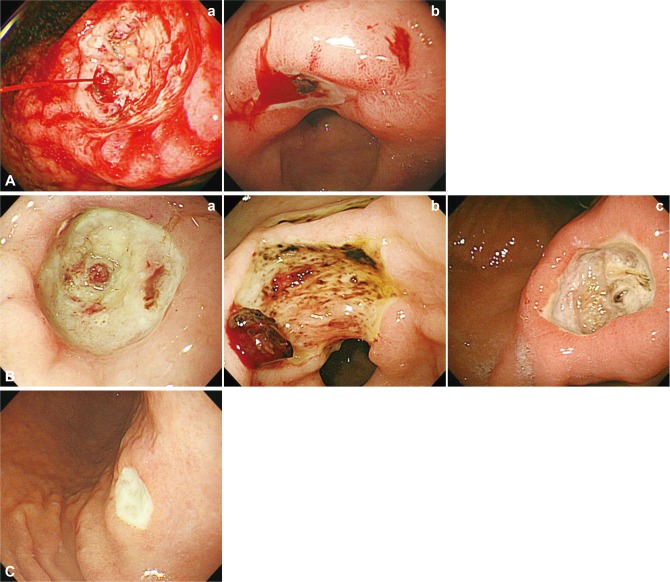
Forrest classification can be summarized as grade: (Aa) Arterial hemorrhage ("spurting"). (Ab) Diffuse hemorrhage ("oozing"). (Ba) Non-bleeding visible vessel. (Bb) Adherent clot. (Bc) Flat pigmented spot. (C) Ulcer without recent stigmata of bleeding ("clean base").
Thermocoagulation, clips or sclerosant injection are recommended alone or in combination with epinephrine injection. Although epinephrine therapy alone is more effective than medical therapy, it is inferior to other monotherapies or combination herapies.19-22
Second-look endoscopy, which is generally defined as a repeat endoscopy within 24 hours after initial endoscopy and hemostatic therapy, is not routinely recommended after endoscopic hemostasis. Several data reported a small but significant reduction in rebleeding in patients undergoing second-look endoscopy,23,24 but these studies were done before high-dose IV PPI therapy have been adopted as the current standard after endoscopic therapy, which suggest that second-look endoscopy may not provide additional benefits.25 However, a subgroup of patients with particularly high-risk presentations may benefit from second-look endoscopy, but this requires further study.
MEDICAL THERAPY AFTER ENDOSCOPY
After endoscopic management, an IV bolus followed by infusion of high-dose PPI reduces recurrent bleeding, need for repeated endoscopy, surgery and blood transfusion. This was evident in the Cochrane meta-analysis, which showed that even mortality was reduced with the use of IV high-dose PPIs.26 The use of high-dose IV PPIs has also been found to be cost effective in both Asia and USA.19,27 However, in patients with lower risk stigmata (clean base, flat pigmented spot), standard PPI therapy (e.g., oral PPI once-daily) is enough to heal the ulcer.15
OTHER CONSIDERATIONS
When the first endoscopy fails to control peptic ulcer bleeding, surgery offers a better chance to secure hemostasis but repeated endoscopic treatment carries fewer complications.28 Angiographic embolization should be considered as an alternative to surgery because not all patients are suitable candidates for surgery.29
LONG-TERM PREVENTION OF RECURRENT BLEEDING ULCERS
Patients with H. pylori-associated bleeding ulcers should receive H. pylori therapy. A systematic review of studies assessing rebleeding in patients with documented H. pylori eradication revealed a 1.3% incidence of rebleeding over a mean follow-up periods of 11 to 53 months.30 After documentation of eradication, maintenance of antisecretory therapy is not needed unless the patient also requires administration of NSAIDs or antithrombotics.
In patients with NSAID-associated bleeding ulcers, the need for NSAIDs should be carefully assessed and NSAIDs should not be resumed if possible. In patients who must restart NSAIDs, a COX-2 selective NSAID plus PPI offers the best available upper gastrointestinal (GI) protection.31,32 The need for antiplatelet therapy should be reviewed in patients who have ulcer bleeding while taking low-dose aspirin. In patients who are taking aspirin for primary prophylaxis (no overt cardiovascular disease), the benefit of low-dose aspirin is relatively small.33 However, the benefit of low-dose aspirin for secondary prophylaxis in patients with established cardiovascular disease is much larger.33 Discontinuing antiplatelet treatment in patients with high cardiothrombotic risk increases the likelihood of occurrence of adverse cardiovascular events. A prospective study in Asia showed that patients whose aspirin treatment was discontinued after endoscopic hemostasis of ulcer bleeding had a lower risk of recurrent bleeding but significantly higher mortality, most of which were related to cardiovascular and cerebrovascular death.34 Thus, it is recommended that aspirin be resumed as soon as possible after achieving endoscopic hemostasis. Data are lacking regarding the optimal timing for resuming clopidogrel or dual antiplatelet treatment after GI bleeding.
CONCLUSIONS
Management of patients with non-variceal UGIB should proceed in a step-wise manner. After initial assessment of hemodynamic status and resuscitation, patients can be risk stratified by clinical features. Most patients should receive an upper endoscopy within 24 hours, and those with high-risk findings on endoscopy should receive endoscopic therapy with IV PPI infusion. Prevention of recurrent bleeding is based on the presumed etiology of the bleeding ulcer. It is recommended that H. pylori should be eradicated if present and NSAIDs should be stopped whenever possible. Patients with established cardiovascular risk should resume antiplatelet therapy as soon as possible after hemostasis.
Notes
The authors have no financial conflicts of interest.