Lower Gastrointestinal Bleeding: Is Urgent Colonoscopy Necessary for All Hematochezia?
Article information
Abstract
Lower gastrointestinal bleeding (LGIB) is defined as acute or chronic abnormal blood loss distal to the ligament of Treitz. The incidence of LGIB is only one fifth of that of the upper gastrointestinal tract and is estimated to be 21 to 27 cases per 100,000 adults per year. Acute bleeding is arbitrarily defined as bleeding of <3 days' duration resulting in instability of vital signs, anemia, and/or need for blood transfusion. Chronic bleeding is defined as slow blood loss over a period of several days or longer presenting with symptoms of occult fecal blood, intermittent melena, or scant hematochezia. Bleeding means that the amounts of blood in the feces are too small to be seen but detectable by chemical tests. LGIB is usually chronic and stops spontaneously. Bleeding stop (80%), but male gender and older patients suffer from more severe LGIB. The optimal timing of colonoscopic intervention for LGIB remains uncertain. Urgent colonoscopy may serve to decrease hospital stay. However, urgent colonoscopy is difficult to control, and showed no evidence of improving clinical outcomes or lowering costs as compared with routine elective colonoscopy.
INTRODUCTION
Urgent colonoscopy is usually performed within 12 to 48 hours of hospitalization. Emergent and urgent colonoscopies, which are performed for variable causes, would be available at only a few hospitals, because urgent colonoscopy requires rapid bowel preparation and experienced endoscopists waiting at all times. In this article, we will discuss the indications and preparation of emergency colonoscopy in patients with lower gastrointestinal bleeding (LGIB).
LGIB
LGIB is defined as acute or chronic abnormal hemorrhage distal to the ligament of Treitz. The incidence of LGIB is only one fifth of that of the upper gastrointestinal tract and is estimated to be 21 to 27 cases per 100,000 adults per year.1,2 Acute bleeding is arbitrarily defined as bleeding of <3 days' duration resulting in instability of vital signs, anemia, and/or need for blood transfusion. Chronic bleeding is defined as slow blood loss over a period of several days or longer presenting with symptoms of occult fecal blood, intermittent melena or scant hematochezia. Occult bleeding means that the amount of blood in the feces are too small to be seen but detectable by chemical tests.3 LGIB usually is chronic and the bleeding stops spontaneous (80%), but male and older patients suffer from more severe LGIB.
The indications of urgent colonoscopy are classified into three categories, with the most common cause being acute LGIB. Urgent Colonoscopy is also performed in patient with colon obstruction due to colon cancer, volvulus or Ogilvie syndrome. Colonoscopy should be avoided, however, for peritonitis, acute colitis and in patients with acute myocardial infarction or pulmonary thrombosis history.
URGENT VERSUS ELECTIVE COLONOSCOPY FOR LGIB
The ideal diagnostic evaluation for patients hospitalized with LGIB is uncertain. After exclusion of an upper GI source, colonoscopy is commonly recommended as the initial diagnostic test for evaluation of LGIB.4
Urgent colonoscopy for acute LGIB has attracted substantial consideration because it allows rapid diagnosis and may lead to appropriate treatment.5-8 Recent studies have shown that colonoscopy, particularly when performed early (within 12 to 24 hours of admission), is safe and effective.9 However, available data suggest that therapy often is not possible and may not be effective when performed.6,9-11
Many therapeutic interventions are available in combination with colonoscopy. It is an efficient and probably cost-effective approach to most patients with LGIB. Early colonoscopy has been shown to reduce the length of hospital stay, independent of other factors, such as severity of bleeding and comorbid illness.12,13 A single previous randomized trial conducted inpatient colonoscopy on 144 patients (57%): 14 were done within <12 hours, 55 in 12 to 24 hours, 46 in 24 to 48 hours, and 29 in >48 hours. After controlling for the other independent correlates, earlier colonoscopy was significantly associated with a shorter length of hospital stay (hazards ratio [HR], 2.02; 95% confidence interval [CI], 1.5 to 2.6; p< 0.0001). The absence of visible blood or active bleeding at the time of colonoscopy was also independently related to a shorter length of hospital stay (HR, 1.5; 95% CI, 1.1 to 2.0; p=0.01).7
Another prior randomized trial of 100 patients assessed urgent colonoscopy (performed within 8 hours of hospitalization or diagnosis of hematochezia) versus standard care (elective colonoscopy within 4 days of admission for patients without continuous bleeding; red blood cell scintigraphy for patients with continuous bleeding, with angiography done for positive studies; and elective colonoscopy within 4 days of admission after negative scintigraphy or angiography).14 The primary end point, rebleeding, was not significantly different between the urgent and standard care groups, which was true for both early rebleeding in hospital (22% vs. 30%; difference, -8%; 95% CI, -25% to 10%) and late rebleeding (16% vs. 14%; difference, 2%; 95% CI, -12% to 16%). No significant differences were identified in transfusions (4.2 units vs. 5.0 units), hospital days (5.8 vs. 6.6), surgery (14% vs. 12%), or mortality (2% vs. 4%).14 Another randomized study also assessed urgent colonoscopy. Eighty-five eligible patients had urgent upper endoscopy; 13 (15%) had an upper source. The remaining 72 were randomized to urgent (n=36) or elective (n=36) colonoscopy. Further bleeding occurred in eight (22%) versus five (14%) of the urgent versus elective groups (difference, 8%; 95% CI, -9% to 26%). Units of blood (1.5 vs. 0.7), hospital days (5.2 vs. 4.8), subsequent diagnostic or therapeutic interventions for bleeding (36% vs. 33%), and hospital charges ($27,590 vs. $26,633) also were not lower in the urgent group. Use of urgent colonoscopy in a population hospitalized with serious lower GI bleeding showed no evidence of improved clinical outcomes or lower costs as compared with routine elective colonoscopy.15 Another single center study reported colonoscopy timing. A total of 50 patients were randomized to each group. A definite source of bleeding was found more often in urgent colonoscopy patients (diverticula, 13; angioectasia, four; colitis, four) than in the standard care group (diverticula, eight; colitis, three) (the odds ratio for the difference among the groups was 2.6; 95% CI, 1.1 to 6.2). In the urgent colonoscopy group, 17 patients received endoscopic therapy; in the standard care group, 10 patients had angiographic hemostasis. There was no difference in outcomes among the two groups-including: mortality 2% versus 4%, hospital stay 5.8 days versus 6.6 days, intensive care unit stay 1.8 days versus 2.4 days, transfusion requirements 4.2 units versus 5 units, early rebleeding 22% versus 30%, surgery 14% versus 12%, or late rebleeding 16% versus 14% (mean follow-up of 62 and 58 months).14 According to above results from studies, we proposed approach algorithm of LGIB (Fig. 1).
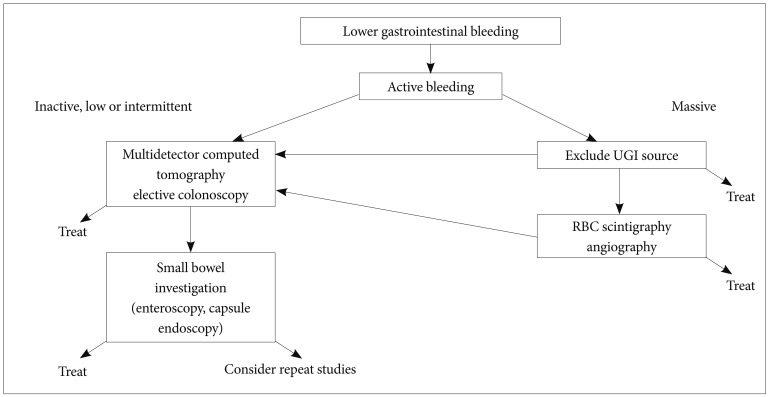
Proposal approach of lower gastrointestinal bleeding. UGI, upper gastrointestinal; RBC, red blood cell.
Because most LGIB is self-limiting, colonoscopy is performed after the bleeding has stopped and the patient adequately prepared. But urgent colonoscopy is performed for continuous bleeding. Signs of hemodynamic instability are pallor, fatigue, palpitations, chest pain, dyspnea, tachypnea, and tachycardia. Especially when standing systolic blood pressure decreased more than 10 mm Hg or heart rate increased more than 10 times per minute, it means more than 15% of the effective blood loss. When hemodynamic instability sign were present, central venous catheter was inserted before a colonoscopy should be performed. Also emergency laboratory test was needed including complete blood count, electrolyte tests, blood clotting, and blood type tests. We needed nonsteroidal anti-inflammatory drugs (NSAIDs) or antiplatelet history and performed digital rectal examination to confirm the appearance of stool and anorectal diseases. Before starting colonoscopy, history and clinical examination should lead to a tentative diagnosis in order to plan the diagnostic procedures. In fact, it is generally accepted that in patients with hematochezia, especially in combination with hemodynamic instability, an upper gastrointestinal bleeding must be excluded, since 12% of patients with suspected acute LGIB have their bleeding source proximal to the ligament of Treitz.4 If a patient presents with bleeding in nasogastric tube aspiration, NSAID or gastric ulcer history and massive bleeding, emergency gastroscopy should be performed. When there are no risk factors of upper gastrointestinal bleeding, colonoscopy is performed. If there are not specific findings in colonoscopy, esophagogastroduodenoscopy may be performed, which allows rapid diagnosis of bleeding, endoscopic intervention and prediction of the risk and site of rebleeding. Therefore, it may reduce duration and cost of hospitalization.16-18 In addition, doctors and patients may benefit from not having to worry about colorectal cancer.
In patients with chronic LGIB, it is the principle to perform colonoscopy selectively after appropriate colonic preparation. However, early colonoscopy can be performed in patients with acute LGIB after hemodynamic instability correction. Some studies reported colonoscopy without preparation,19 although it may cause difficulty in finding the bleeding site and increase the risk of perforation. In other studies, the detection rate of the bleeding source after bowel preparation varies between 62% and 78% and, in patients without preparation, the urgent colonoscopy without bowel preparation could identify the bleeding source in 76%. It is unclear whether colonoscopy without bowel preparation is more effective compared to colonoscopy with bowel preparation with only few randomized controlled trials on the subject; however, most endoscopists prefer prepared colonoscopy.7,20 The bowel preparation can be performed by enemas and/or polyethylene glycol (PEG) solutions administered by mouth or both. PEG solution is administered 1 L every 30 to 45 minutes by orally or nasogastric tube and administered to maintain the colon preparation average of 5.5 L (range, 4 to 14). Metoclopramide 10 mg administered intravenously may be helpful in improving gastric emptying and reducing nausea.16 Narcotic analgesics can temporarily reduce mucosal blood flow, making it difficult to find such as angiodysplasia. Therefore, it is not recommended in patients with LGIB.
CONCLUSIONS
Patients presenting with clinically serious hematochezia should undergo upper endoscopy initially to rule out an upper GI source. The optimal timing of colonoscopic intervention for LGIB remains uncertain. The use of urgent colonoscopy in patients with serious LGIB showed no evidence of improving clinical outcomes or lowering costs as compared with elective colonoscopy. Most patients had no further bleeding in the hospital and did not undergo further diagnostic or therapeutic interventions for bleeding. However, we need to tailored approach in patients with acute LGIB.
Notes
The author has no financial conflicts of interest.