Endoscopic Management of Peptic Ulcer Bleeding
Article information
Abstract
Acute upper gastrointestinal bleeding is a common medical emergency around the world and the major cause is peptic ulcer bleeding. Endoscopic treatment is fundamental for the management of peptic ulcer bleeding. Despite recent advances in endoscopic treatment, mortality from peptic ulcer bleeding has still remained high. This is because the disease often occurs in elderly patients with frequent comorbidities and are taking ulcerogenic medications. Therefore, the management of peptic ulcer bleeding is still a challenge for clinicians. This article reviews the various endoscopic methods available for management of peptic ulcer bleeding and the techniques in using these methods.
INTRODUCTION
Acute upper gastrointestinal bleeding (UGIB) is defined as bleeding arising from a lesion proximal to the ligament of Treitz.1 Peptic ulcer bleeding (PUB) is reported to be the most common cause of UGIB.2 The incidence of PUB is reported to be from 19.4 to 57 per 100,000 population per year.3 The mortality rate from PUB is reported to be from 2.5% to 5.8%.4,5,6 In United Kingdom, surgery for PUB has continued to decrease from 8% to 2% between 1993 and 2006.2,7 In the USA, admissions to hospitals for PUB decreased by 28.2% and the use of endoscopic treatment increased by 58.9% between 1993 and 2006.8 In Korea, an early study reported that the average age of patients with PUB increased from 50.8 to 56.5 years between 1993 to 1995 period and 2000 to 2002 period.9 The rate of endoscopic treatment increased from 17.6% to 39.0% and the rate of surgery decreased from 11.5% to 5.2% during this period. However, the overall mortality rate increased from 5.4% to 7.7% during this period. This is because the disease often occurs in elderly patients with frequent comorbidities and are taking ulcerogenic medications. Currently, most of the studies on the epidemiologic data on PUB have been published from Western countries. Although peptic ulcer disease is common in Korea, the prevalence of PUB has not been well studied. This review focuses on the endoscopic management of PUB. Pre-endoscopic assessment, resuscitation and postendoscopic management are beyond the scope of this review and is not touched upon in this review.
ENDOSCOPIC MANAGEMENT OF PUB
Pre-endoscopic period
Complete visualization of the stomach may not be possible in patients with PUB due to stomach contents and blood. A clear endoscopic field is essential for the success of endoscopic hemostasis. Prokinetic drugs such as erythromycin and metoclopramide given before endoscopy were expected to improve visualization. However, the results of currently published studies are disappointing. A recent meta-analysis found that prokinetic drugs reduced the need for a second endoscopic examination; however, there was no difference in need for transfusion, hospital stay, and surgery.10 However, only three full text articles were included in this meta-analysis and currently there is not enough evidence regarding the use of prokinetics in patients suspected with PUB.
When to perform endoscopy
Endoscopy is essential for the diagnosis of the cause of bleeding and endoscopic treatment can reduce re-bleeding, surgery, and mortality.11 Although the role of endoscopy is obvious in PUB patients, when to perform endoscopy is not yet clarified. The majority of data published suggest that early endoscopy (generally defined as endoscopy within 24 hours) is safe and can reduce transfusion requirements and length of hospital admission.12 However, no mortality benefit could be identified with early endoscopy. Several studies have investigated the efficacy of urgent endoscopy (endoscopy performed with 6 or 12 hours) compared with elective endoscopy.13,14,15 The results of these studies suggest that urgent endoscopy can reduce hospital stay and amount of blood transfusion. However, outcomes of recurrent bleeding, surgery, and deaths were not associated with urgent endoscopy. Based on these results, early endoscopy within 24 hours seems to be mandatory for patients with PUB while urgent endoscopy within 1 to 4 hours is recommended for patients with clinical evidence of continued bleeding.
When to treat PUB
The Forrest classification is most widely used to classify the endoscopic appearance of bleeding peptic ulcers.16 Nowadays it is widely used to predict the risk of re-bleeding and mortality and is known to have a stronger association with gastric ulcers compared with duodenal ulcers.17,18,19 The Forrest classification classifies ulcers with a spurting hemorrhage (Forrest Ia), an oozing hemorrhage (Forrest Ib), a visible vessel (Forrest IIa), an adherent clot (Forrest IIb), hematin on the ulcer base (Forrest IIc), and a clean ulcer base (Forrest III).19
Endoscopic treatment is mandatory for ulcers with active bleeding or with a non-bleeding visible vessel.20 Endoscopic treatment is generally not recommended for ulcers with hematin on the ulcer base or a clean ulcer base.20 Controversy exists whether ulcers with an adherent clot need endoscopic treatment, but treatment is generally recommended when the clot is resistant to vigorous irrigation.20
METHODS OF ENDOSCOPIC TREATMENT
Injection therapy
Endoscopic treatment can be divided into injection, thermal, and mechanical methods. Injection therapies consists of epinephrine (Fig. 1), sclerosants (absolute ethanol, polidocanol), and tissue adhesives (thrombin/fibrin glues). Injection of epinephrine is the most widely used method for hemostasis. It is easy to perform and requires less coordination between the endoscopist and the assistant compared to other methods. Epinephrine injection is effective at achieving initial hemostasis mainly due to a tampon effect.1 However, epinephrine monotherapy is less effective than other monotherapies such as electrocoagulation, clips, or fibrin glues in preventing further bleeding.21 Also, adding a second modality such as electrocoagulation or clips is significantly more effective than epinephrine alone in reducing further bleeding and surgery.21 It is now widely considered that epinephrine monotherapy is inadequate and should be combined with another modality. In clinical practice, injection of epinephrine is generally performed before other therapies in order to slow or stop bleeding which allows improved visualization for subsequent therapies.20 The optimal volume of epinephrine injection is not known; however, diluted solutions (1:10,000 or 1:20,000) are injected in 0.2 to 2 mL aliquots in all four quadrants of the bleeding stigma. Sclerosant injection significantly reduces further bleeding when compared with no endoscopic therapy.21 However, sclerosants such as alcohol is not routinely used for treatment of bleeding peptic ulcers, possibly due to concerns for tissue necrosis. Absolute alcohol can be administered in 0.1 to 0.2 mL aliquots with limitations of 1 to 2 mL due to concerns of tissue injury.22
Thermal therapy
Thermal contact therapy can be classified into contact or noncontact methods. Contact methods consists of heater probe or bipolar electrocoagulation and noncontact methods consist of argon plasma coagulation (Fig. 2).23 Thermal methods are significantly effective in achieving initial hemostasis, reducing further bleeding, surgery, and mortality.21 Currently, no significant difference has been found between the different thermal modalities. Two studies reported that epinephrine injection followed by thermal therapy was more effective than thermal therapy alone.24,25 Thermal contact therapy should be performed with the tip of the probe as close as possible to the bleeding ulcer. Endoscopic caps may be used to improve visualization and access for therapy.26 When available, use of soft caps is preferred to minimize contact bleeding.
Mechanical therapy
Clips have been found to be more effective than epinephrine injection in reducing further bleeding and surgery but less effective than thermal therapy (Fig. 3).21 Clips likely do not induce tissue injury which would be a benefit over thermal therapies and sclerosants. However, clips are not currently reimbursed by the Korean National Health Insurance and is generally considered to be more expensive than the other hemostatic methods. Also, training the assistants in handling of the clip is needed for successful application. Another limitation of endoclips is that it is difficult to apply in fibrotic lesions.27 Also, currently used endoclips allow for only single clip deployment and in cases where multiple clips are necessary, repeated passage of the device may prolong the procedure time. When using an endoclip, the clip and the target should be close to the endoscope for better control of the clip. In order to capture maximal amount of tissue around the lesion, suction can be applied before deployment.27 Precise placement of the first endoclip is crucial as improper placement can prevent the proper placement of additional clips.

Endoscopic findings. (A) A spurting was observed at duodenal ulcer. (B) A spurting was stopped by apply of endoclip.
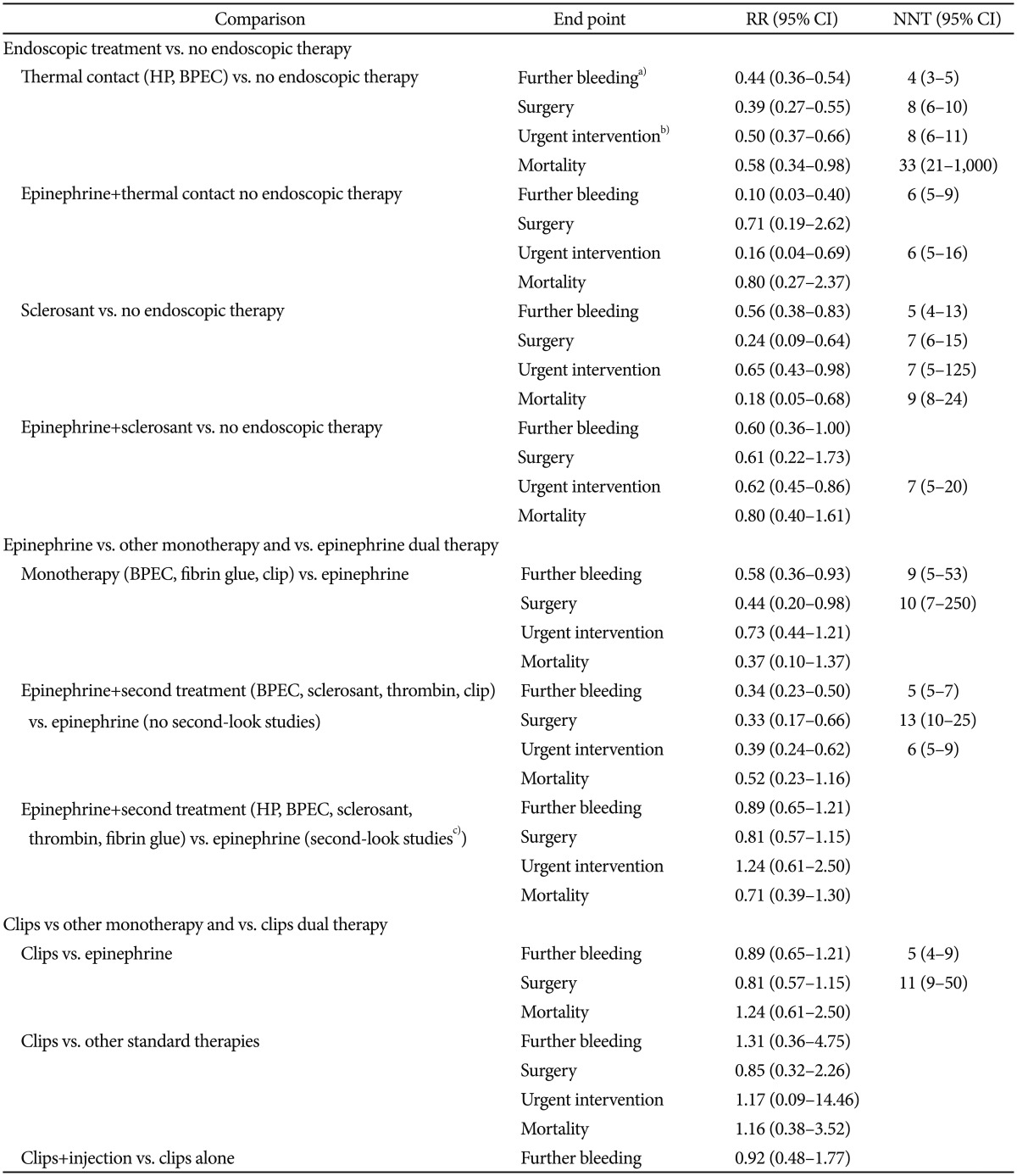
Laine and McQuaid21 reported meta-analyses for endoscopic treatment methods on bleeding ulcers. The results were summarized in Table 1.
POSTENDOSCOPIC PERIOD
Second look endoscopy
Second look endoscopy is defined as routine endoscopy after initial hemostatic therapy. According to recent guidelines, routine second look endoscopy after initial endoscopic hemostasis is not recommended and should be reserved for patients with high risk of re-bleeding.20 This is because high dose intravenous proton pump inhibitor was shown to be as effective as second look endoscopy in reducing re-bleeding.28 However, there is no grading system that can reliably classify patients who are at high risk of re-bleeding and further studies are needed in this aspect.29
Continued and recurrent bleeding
Endoscopic hemostasis is not successful in 8% to 15% of patients.1 The re-bleeding rate of patients with ulcers is dependent on factors such as size, depth, location, concurrent medical comorbidities, severe coagulopathies, presentation with shock or hypotension, and start of bleeding as an inpatient.30 Most of the re-bleeding episodes are reported to occur in the first 7 days.31,32 Patients who fail to achieve hemostasis by endoscopic measure should receive angiographic embolisation. When compared to surgery, angiographic embolisation is associated with reduced complications but with higher re-bleeding rates.33,34,35,36,37
Recurrent bleeding occurring after initial successful endoscopic hemostasis can be treated by repeated endoscopic treatment. When compared to surgery, repeated endoscopic treatment achieves comparable hemostasis with substantially less postoperative complications.38 Risk factors reported to be associated with re-bleeding are nonsteroidal anti-inflammatory drug use, ulcer size, age, genetic components, anticoagulant use, shock, and low blood pressure.3 Currently, a nationwide cohort investigating the risk factors associated with re-bleeding after PUB in Korea is ongoing.
CONCLUSIONS
The epidemiology of PUB has changed and patients with PUB presents at an older age with increased comorbidities. Despite advances in pharmacology and endoscopic techniques, the mortality rate of PUB seems to be similar partly due to this change in epidemiology. Endoscopy remains the mainstay of treatment for patients with PUB. Among the various hemostatic methods, epinephrine injection should be combined with another modality. The benefits of routine second look endoscopy seem to be minimal and patients who fail to achieve initial hemostasis should receive angiographic embolisation.
Notes
Conflicts of Interest: The authors have no financial conflicts of interest.