Endoscopic Management of Anastomotic Strictures after Liver Transplantation
Article information
Abstract
Endoscopic treatment of biliary strictures involving plastic stent placement has been used widely. The use of self-expandable metal stents (SEMSs) has been described for anastomotic strictures following liver transplantation (LT). This review aimed to assess and compare the efficacy of plastic stents with SEMS in LT patients. Information was retrieved regarding technical success, stricture resolution, the number of endoscopic retrograde cholangiography procedures, follow-up, immediate, and late complications. Eight studies involving plastic stents had a stricture resolution rate of 84.5%, with the rates ranging from 63% to 100%. These rates are comparable with the stricture resolution rate of 75% determined from six studies that involved 236 patients who received metal stents and the rates ranged from 53% to 81%. The observed success rate for metal stents used to manage post-LT anastomotic biliary strictures was below the reported rate for multiple plastic stents. Hence, the currently available metal stents should not be offered for the management of post-LT anastomotic biliary strictures.
INTRODUCTION
Liver transplantation (LT) is a final treatment option for patients with chronic end-stage liver disease or acute liver failure when medical and surgical treatments are not possible [1]. Since Starzl et al. [2] first performed a LT in 1963, the current overall 1-year survival for deceased donor LTs has reached 85%, which is a consequence of continuous advances in organ selection, retrieval, preservation, and implantation techniques [3].
However, a range of complications can develop following LT, and biliary complications, including strictures, bile leaks, and stones are important causes of morbidity and mortality in LT recipients [4], and biliary strictures are observed in about 32% of post-orthotopic LT patients [4]. Until recently, surgery has been the standard of care for the treatment of biliary strictures in post-LT recipients, but the diversification of endoscopic accessories and the accumulated experience in endoscopic treatment have tended to postpone surgery until endoscopic treatment fails [5,6].
Biliary strictures are classified into two major categories, namely, non-anastomotic strictures (NASs) and anastomotic strictures (ASs). NASs account for about 20% to 25% of stricture complications that follow orthotopic LTs, and they generally present as multiple, long segment strictures [7]. On the other hand, ASs occur in about 5% to 10% of LT recipients within 1 year of surgery, and they are mainly localized within the anastomosis sites, and, compared with NAS, they are relatively short [8]. Thus, the endoscopic treatment success rates are higher for ASs [4].
ENDOSCOPIC MANAGEMENT OF ANASTOMOTIC STRICTURE
Standard method for endoscopic retrograde cholangiography
If an AS is detected, the degree and length of the stricture can be managed during endoscopic retrograde cholangiography (ERC). To this end, the guidewire is positioned at the bile duct of the proximal site past the stricture, then the stricture site is balloon dilated and an endoscopic retrograde biliary drainage (ERBD) stent is inserted [9]. This method has been repeatedly reported to be more effective than performing a balloon dilatation alone [10-12]. The balloon must be slowly inflated to the size of the donor’s bile duct only or the Soehendra biliary dilation catheter (SBDC) is sometimes used for dilation. If the stricture is too constricted to allow the balloon catheter or SBDC to advance, the Soehendra stent retriever can be used [13]. Then, a plastic stent is inserted. Based on our review, the treatment of most patients with AS requires balloon dilatations of 4 to 10 mm for 30 to 60 seconds and a 7- to 10-Fr ERBD stent [4,14,15].
Endoscopic retrograde cholangiography protocol and its variations
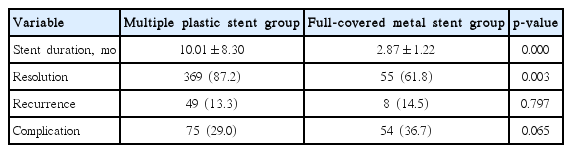
ERC must be repeated every 3 months to examine the dilatation of the stricture site and minimize the risk of stent occlusion as well as the risks of inducing cholangitis or stones in the superior segment of the stricture [9,12]. Furthermore, every time ERC is performed, greater numbers of stents with greater diameters must be placed at the stricture to maximize the effects of dilatation [16]. During follow-up ERCs, the previously inserted stents are removed using a polypectomy snare or forceps. If the cholangiogram shows a patent AS, the treatment is terminated. If not, the dilatation and stent insertion are repeated. As yet, a consensus has not been reached regarding the optimal number of plastic stents. Several reports have described the use of two to four plastic stents to treat AS, and the average number of plastic stents used is 2.80 (Table 1) [15-23].
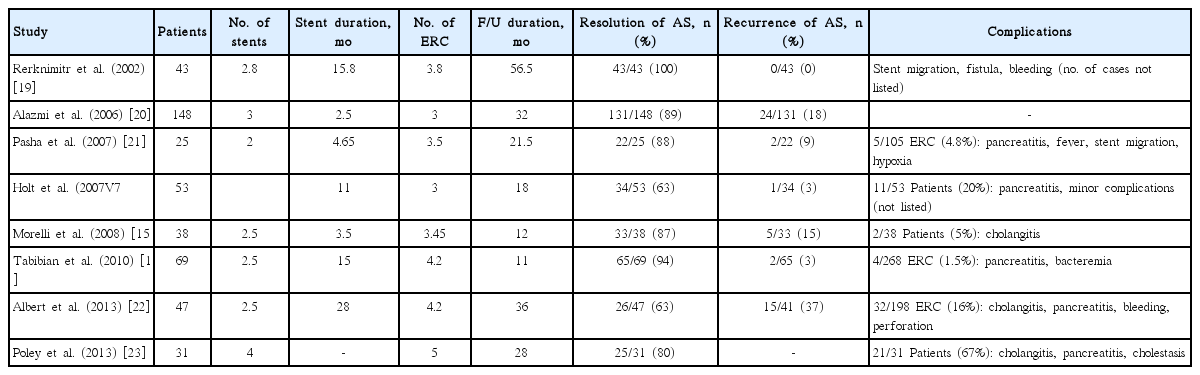
Data from Multiple Plastic Stents Insertion for Treatment of Anastomosis Stricture after Liver Transplantation
Yazumi et al. [24] did not insert an ERBD stent and they only performed balloon dilatation during the first ERC. These investigators suggested that an ERBD stent should be inserted only when a residual stricture is observed during the follow-up ERC [24]. However, Hsieh et al. [25] recently described a method for the balloon dilatation of a stricture site to a diameter that was as wide as the intrahepatic bile duct that enabled the insertion of as many plastic stents as possible and produced outstanding therapeutic outcomes. In addition, other methods have been described that involve inserting as many plastic stents as possible during the first ERC [26] and rapid-sequence ERC management in which ERC is performed at 2-week intervals to treat the stricture [15].
If AS is observed within a few days of the LT or there are concomitant bile leaks, a gradual dilatation is safer. On the other hand, rapid and aggressive dilatations can be considered for patients with AS a few months after LT to shorten the total treatment duration [24].
Types of endoscopic retrograde biliary drainage stents
Plastic (polyethylene) stents are undoubtedly the most popular ERBD stent. They are easily inserted into the stricture site, inexpensive, and they are easily replaceable. However, they are associated with an increased risk of stent occlusion because of their relatively small diameters. Thus, multiple side-by-side plastic stent insertions are widely performed. Unfortunately, this method requires multiple ERC sessions, which increase the burden on patients and potential complications, including pancreatitis and perforation [27].
Self-expandable metal stents (SEMSs), which have larger diameters, have been introduced to address these problems [4]. SEMSs can be classified into the covered and uncovered types. When inserted, uncovered SEMSs infiltrate into the submucosal layer over time, resulting in mucosal hyperplasia and ingrowths. This, in turn, hinders stent removal and it narrows the diameter of the SEMS, eventually inducing SEMS occlusion and stone formation [28]. As removing these stents is very challenging and it increases the risk of complications, such as infection, bleeding, and perforation, they should not be used for AS [29,30].
Consequently, covered SEMSs are more popular for this patient population. The patency of covered SEMSs maintained for relatively long periods because the outer coating prevents tissue ingrowths, and the SEMSs can be removed relatively simply and safely using a snare or rat tooth forceps [28]. The partially covered SEMS, which is a modified version of the covered SEMS, has limitations with respect to long-term efficacy [31]. Indeed, covered SEMSs induce strictures at the uncovered proximal and distal ends [32].
SEMSs with diameters of up to 10 mm are currently used, and they are about three-time wider than plastic stents. Therefore, SEMSs may maintain their patency. However, as previously described, a stepwise increase in the number of plastic stents ultimately produces stricture dilatation of a similar degree as that produced by SEMS placement. To produce such effects, however, ERC has to be performed several times at regular intervals. In this context, this study reviewed all of the literature that describes the treatment of AS using multiple plastic stents (MPS) or covered SEMS to examine the features and clinical efficacy of each stent type. We estimated the numbers of patients based on the demographic data, the stricture resolution rates, the recurrence rates, and the complication rates, and we analyzed the data using the chi-square test and independent sample t-test with SPSS version 15 (SPSS Inc., Chicago, IL, USA). The differences were considered significant when the two-sided p-value was <0.05.
Multiple plastic stent vs. covered self-expandable metal stent
Stent insertion durations
The stent insertion durations ranged from 2.5 to 28 months in the MPS group and from 2 to 5.5 months in the SEMS group (Tables 1, 2). However, when the aforementioned rapid-sequence ERC protocol was applied to the MPS group, the stent insertion duration was 3.5 months, which was similar to the average insertion duration in the SEMS group (Table 3).

Data from Full-Covered Metal Stent Insertion for Treatment of Anastomosis Stricture after Liver Transplantation
Stricture resolution rates
Among the publications that describe the use of MPS, the best performance reported was a stricture resolution rate of 100% (Table 1). Among the studies that used covered SEMS, the study by Traina et al. [33] had the best success rate, with an 81% stricture resolution rate (Table 2). Stricture resolution was confirmed in the eight studies in which MPSs were used, indicating a success rate of between 63% and 100%. On the other hand, stricture resolution was confirmed in the five studies in which covered SEMSs were used, indicating a success rate of between 53% and 81%. Indeed, the average success rates were 87.2% in the MPS group and 61.8% in the SEMS group; hence, the SEMS group had a significantly lower success rate (p=0.003) (Table 3).
Stricture recurrence rates
After achieving stricture resolutions, the stricture recurrence rate ranged from 0% to 37% after MPS treatment (Table 1). On the other hand, the stricture recurrence rate after treatment with covered SEMS ranged from 7% to 25% (Table 2). The average stricture recurrence rates were 13.3% (49 of 369 patients) in the MPS group and 14.5% (eight of 55 patients) in the covered SEMS group, a difference that was statistically insignificant (p=0.797) (Table 3).
Complication rates
The postoperative complications varied greatly, and they included post-ERC pancreatitis, cholangitis, bleeding, pain, and ERBD stent migration. As predicted, stent migration was rarely reported in the MPS group, but it accounted for between 4% and 46% of all of the complications in the covered SEMS group (Table 2) [33-37]. In addition, post-SEMS placement pain was relatively transient, and was easily treated with analgesics for a short period. Overall, with the exception of one report, the incidence of complications in the MPS group was below 20%, while that in the covered SEMS group was between 26% and 44%. Hence, a higher incidence of complications was indicated in the covered SEMS group compared with that in the MPS group. The average complication rates were 29.0% in MPS group and 36.7% in SEMS group. Complications developed more frequently in the SEMS group (p=0.065) (Table 3).
CONCLUSIONS
Biliary plastic stents have undergone continual improvements and changes since they were first introduced in 1979 [38]. One persistent weakness is their short-lived patency caused by their small diameters. Technically speaking, a wider plastic stent could be fabricated, but a plastic stent that is larger than 12 Fr cannot be placed within the bile duct because of limitations in the size of a duodenoscope’s working channel. Therefore, with the exception of patients who require simple biliary drainage, a plastic stent with a small diameter is not preferred for patients whose strictures must be widened mechanically, including those with post-LT AS, which inevitably require multiple rounds of ERC.
This is the main reason underlying the increase in the popularity of SEMS for treating AS. However, using a covered SEMS increases the risk of stent migration, which undermines its therapeutic effects by hindering stent placement for the desired period. The use of partially covered SEMSs for the treatment of AS has been reported; however, they have been associated with strictures at their uncovered portions [31,32]. MPSs boast a high success rate with low complication and recurrence rates for the treatment of AS, thereby further reducing the possibility of covered SEMS superseding MPS as the primary therapeutic modality. A recent report by Tarantino et al. [35] recommended SEMS as a rescue therapy only when AS treatment with MPS has failed.
The recurrence rates were similar in the MPS and SEMS groups. In most the studies that we reviewed, the recurrence of AS was high among those patients who had delayed initial presentations of >6 months and very tight strictures initially. Thus careful monitoring that involves periodic evaluations of the liver enzymes, and ultrasonography and/or magnetic resonance cholangiopancreatography, depending upon the nature and duration of the stricture, is needed after AS resolution.
New biliary bioabsorbable stents are under development. Therefore, new treatment modalities and devices could replace those currently available for the treatment of post-LT AS.
Notes
Conflicts of Interest: The authors have no financial conflicts of interest.