Cracking Difficult Biliary Stones
Article information
Abstract
Apart from difficult biliary cannulation, biliary stone removal is considered one of the hurdles in endoscopic retrograde cholangiopancreatography. Generally, simple common bile duct (CBD) stones can be removed either with an extraction balloon or a basket. However, there are difficult stones that cannot be removed using these standard methods. The most difficult stones are large CBD stones and impacted stones in a tapering CBD. A few decades ago, mechanical lithotripsy was usually required to manage these stones. At present, endoscopic papillary large balloon dilation (EPLBD) of the biliary orifice has become the gold standard for large CBD stones up to 1.5 cm. EPLBD can reduce the procedural time by shortening the stone removal process. It can also save the cost of the devices, especially multiple baskets, used in mechanical lithotripsy. Unfortunately, very large CBD stones, stones impacted in a tapering CBD, and some intrahepatic duct stones still require lithotripsy. Peroral cholangioscopy provides direct visualization of the stone, which helps the endoscopist perform a probe-based lithotripsy either with an electrohydraulic probe or a laser probe. This technique can facilitate the management of difficult CBD stones with a high success rate and save procedural time without significant technical complications.
INTRODUCTON
Since the introduction of endoscopic biliary sphincterotomy in 1974 [1,2], the management of bile duct stones has shifted from surgical bile duct exploration to an endoscopic approach. However, there is a 15% failure rate of bile duct stone removal with standard biliary sphincterotomy plus stone extraction with either a balloon, a basket catheter, or their combination [3]. Stone factors (e.g., size, number, or shape), bile duct factors (e.g., associated stricture, narrowing, or angulation), and the relationship between the stone and the bile duct (e.g., impacted stone) influence the success of stone extraction [4]. The two main principles to facilitate stone removal in this situation are expanding the stone passage and reducing the stone size. Endoscopic papillary large balloon dilation (EPLBD) with a balloon sized ≥12 mm (Fig. 1) can result in up to a 50% reduction in the need for mechanical lithotripsy (ML) [5]. Both the American Society for Gastrointestinal Endoscopy (ASGE) and the European Society of Gastrointestinal Endoscopy (ESGE) recommend the use of EPLBD when dealing with difficult biliary stones [4,6]. Because of safety concerns, EPLBD is contraindicated in the presence of biliary strictures or significantly tapered bile ducts, and the selected balloon size should not exceed the bile duct diameter to reduce the risk of perforation. In addition, the risk of bleeding can be minimized by choosing an adequate balloon inflation time (approximately 60 sec) and avoiding a large sphincterotomy before performing sphincteroplasty [7]. Limited sphincterotomy is recommended before performing EPLBD [6,7]. Notably, the anecdotal concern about the risk of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis after balloon sphincteroplasty has been cleared by a recent meta-analysis showing that EPLBD without prior sphincterotomy did not increase the risk of pancreatitis [8].
A large bile duct stone successfully treated with endoscopic papillary large balloon dilation (EPLBD). (A) Cholangiogram showing a large bile duct stone. (B) Endoscopic view of EPLBD after sphincterotomy. (C) A large stone removed with an extraction balloon. (D) Occlusion cholangiogram showing no residual filling defect.
Despite the use of EPLBD, approximately 30% of stone removal cases remain unsuccessful [9-11]. Therefore, stone-cracking techniques are needed to reduce the stone size before standard stone removal. These techniques include ML, laser lithotripsy (LL), electrohydraulic lithotripsy (EHL), and extracorporeal shock-wave lithotripsy (ESWL). ML, LL, and EHL can be performed in an endoscopy suite; however, LL and EHL require direct visualization of the stone to precisely target and prevent bile duct injury. ESWL requires separate sessions of lithotripsy followed by ERCP for stone-fragment clearance. Practically, temporary biliary stenting is recommended as a bridge before complete stone removal [4].
MECHANICAL LITHOTRIPSY
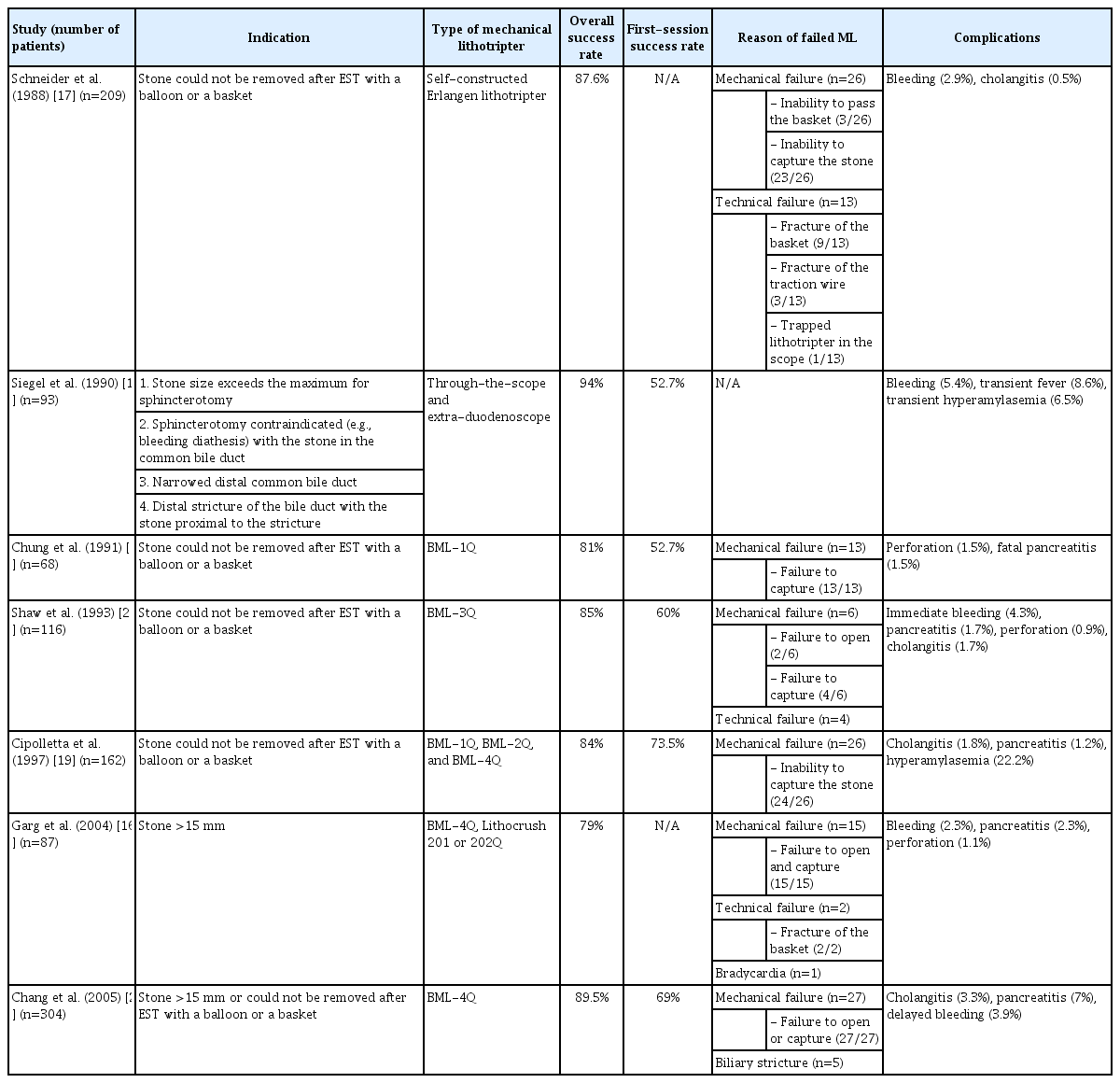
ML uses the shearing force between the basket wire and the metal sheath to crack the stone. The three main elements of a mechanical lithotripter are a basket, a traction wire, and a metal sheath. The stone is captured in the basket and crushed by tension applied to the traction wire. The basket can be used to remove stone fragments [12]. There are two systems for metal sheath application [13]. The first system is an extra-duodenoscope, in which the endoscope is removed after the stone is captured in the basket and the Teflon sheath of the basket is replaced by a metal sheath before lithotripsy [13]. This system can rescue the trapped Dormia basket; therefore, it is also known as an emergency lithotripter [14]. The second system is a self-contained through-the-scope mechanical lithotripter, in which the metal sheath can pass through the accessory channel of the endoscope (Fig. 2). After this system was introduced in 1982 [15], ML has been commonly used for difficult stones, especially those >15 mm or those that could not be removed with a balloon or a basket catheter after an endoscopic sphincterotomy. The overall success rate of ML ranges from 79% to 94%, and the overall complication rate ranges from 3.3% to 17.6% [13,16-21]. However, the stone clearance rate in the first ML session ranges from 52.7% to 73.5% [13,18-21], which means that up to half of the patients require more than one ERCP session. The main reasons for failed ML are (1) inability to capture the stone because the stone size was too large, (2) inability to open the basket because the stone was impacted, and (3) biliary stricture (Table 1). Additionally, technical failures of ML, including a broken basket or a broken traction wire, have been reported to occur at a rate of 3.6%–6% [16,17,21,22].

Mechanical lithotripsy for a difficult bile duct stone. (A) A 1-cm stone proximal to a considerably tapered bile duct. (B) Mechanical lithotripsy was successfully performed using a through-the-scope mechanical lithotripter, and stone clearance was achieved.
CHOLANGIOSCOPY-GUIDED LITHOTRIPSY
Endoscopic EHL and LL for bile duct stones were introduced in 1977 [23] and 1986 [24], respectively. However, the original version of the cholangioscope, the mother-baby cholangioscope, was considered a costly and cumbersome device [25]. After the development of single-operator cholangioscopy (SOC) [26], EHL and LL have gained popularity. Direct visualization is necessary for both EHL and LL to precisely target the stones and prevent bile duct injury. The SOC scope can be inserted through the accessory channel of the duodenoscope. The EHL or LL probe can be inserted through the 1.2-mm channel and, more important, it can be operated by one endoscopist (Fig. 3). A recent meta-analysis of 35 studies (1,762 patients) demonstrated that cholangioscopy-guided intraductal lithotripsy for difficult biliary stones had an overall success rate of stone fragmentation of 91.2%, with 76.9% complete stone clearance in a single session. Notably, the overall adverse event rate was 8.9% [27]. The subgroup analysis between EHL and LL found that there was no difference in the success rates of overall stone fragmentation (90.1% vs. 92.9%, p=0.360). However, EHL had a lower rate of complete stone clearance in a single session (70.9% vs. 83%, p=0.021) and a longer mean procedure time (75.7 min vs. 54.3 min, p<0.001) than LL [27]. Although the authors did not compare the types of cholangioscopes, the newer digital cholangioscope seemed to have a higher success rate and a lower complication rate than the original fiber-optic generation. The overall stone fragmentation success rates of the mother-baby cholangioscope, first-generation SOC scope, and second-generation SOC scope were 89.3%, 90.0%, and 95.0%, respectively. The rates of complete stone clearance in a single session were 66.8%, 80.6%, and 80.4%, respectively, and the overall adverse event rates were 13.5%, 9.8%, and 4.1%, respectively [27]. Data from a large multinational registry demonstrated that a larger size of the largest stone and a higher number of stones had a negative impact on the rate of complete stone clearance in a single session [28].
Laser lithotripsy guided by single-operator cholangioscopy. (A) A disposable cholangioscope operated by a single endoscopist. The laser probe is inserted through the accessory channel of the cholangioscope, which is inserted through the accessory channel of the duodenoscope. (B) Cholangioscopic view of intraductal stone fragmentation with a laser probe.
Cholangioscopy-guided lithotripsy is superior to other methods, including ML or EPLBD, because it can be used as a rescue method after the failure of ML or EPLBD, and is a good alternative to common bile duct (CBD) exploration. Buxbaum et al. reported that SOC-guided LL provided a higher stone clearance rate in >10-mm stones than the conventional methods, including ML and balloon sphincteroplasty (93% vs. 67%, p=0.009), in a randomized study [29]. Another randomized control, non-inferiority study by Franzini et al. demonstrated that SOC-guided EHL had comparable outcomes to EPLBD with respect to the rate of complete stone clearance in a single session (77.1% vs. 72%, p>0.05) and the adverse event rate (4.2% vs. 12%, p>0.05) [10]. However, EPLBD had a significantly shorter procedural time than EHL (47.1 min vs. 72.3 min, p<0.05). Interestingly, in the second session, which was performed using a cross-over technique, EHL had a two times higher stone clearance rate than EPLBD [10]. Another randomized controlled study by Bang et al. demonstrated that SOC-guided LL had a higher rate of complete stone clearance in a single session than EPLBD (93.9% vs. 72.7%, p=0.021), with comparable adverse event rate (9.1% vs. 3%, p=0.61) and overall cost ($16,684 vs. $10,626, p=0.097) [11]. A multiple logistic analysis revealed that single-session success was significantly associated with the use of LL, a stone-to-extrahepatic duct ratio of ≤1, and the absence of a tapered bile duct, defined as a <0.5 ratio of the distal bile duct diameter (measured at 1 cm above the ampullary orifice) to the widest point in the proximal CBD [11]. Furthermore, a randomized study by our group on huge stones with failed EPLBD demonstrated that SOC-guided LL was superior to ML in terms of having a higher rate of stone clearance in a single session (100% vs. 63%, p<0.01) and a lower radiation exposure (20,989 mGycm2 vs. 40,745 mGycm2, p=0.04), whereas the adverse event rates were comparable (6% vs. 13%, p=0.76) [9]. In addition, LL cleared all stones that ML failed to remove, and no surgery was needed in any patient [9]. In a comparison with laparoscopic CBD exploration for >20 mm CBD stones, SOC-guided LL had a lower stone clearance rate in a single session than surgery (83.3% vs. 96.2%, p=0.023). However, the overall stone clearance rates (92.3% vs. 96.2%, p=0.124) and overall adverse events (5.1% vs. 10.1%, p=0.246) were comparable between the two procedures. Interestingly, patients who underwent SOC-guided LL had a shorter hospital stay (5.7 days vs. 8.8 days, p=0.001) and enhanced recovery, as determined by the postoperative gastrointestinal quality of life index at 1 and 3 months, than patients who underwent laparoscopic CBD exploration [30].
Although the cost of disposable SOC scopes is relatively high, it could be a trade-off against multiple sessions of endoscopy (if the stones could not be cleared in a single session) and/or a longer hospital stay (if surgery is needed). A cost-effectiveness study from Belgium demonstrated that SOC-guided lithotripsy (either EHL or LL) reduced the overall expenditure for difficult bile duct stones when compared with ML [31].
Direct peroral cholangioscopy (DPOC) is a procedure in which an ultra-slim upper endoscope is passed through the mouth into the bile duct without a side-viewing duodenoscope. This technique was first reported in 2007 [32]. Despite several adjunct accessories to assist bile duct insertion, such as a super-stiff guide wire [32], a balloon anchor [33], and a special overtube [34], this technique is still not widely used because it is technically demanding. Recently, an ultra-slim endoscope (CHF-Y0010; Olympus Medical Systems, Co., Ltd., Tokyo, Japan; Fig. 4), a new prototype of DPOC with two bending sections in the distal end, two accessory channels (2.2- and 1-mm diameter), and a 4.9-mm-diameter (at the tip) scope, was evaluated [35]. This multibending ultra-slim scope has a higher success rate of free-hand biliary insertion than the conventional ultra-slim scope (89.1% vs. 30.4%, p<0.001), with comparable adverse event rates (6.5% vs. 4.3%, p=0.50) [35]. DPOC-guided lithotripsy was reported to have a high overall stone clearance rate of 84.6%–90%, although the studies included a small number of patients [36-38]. However, when performing endoscopy directly in the bile duct, special caution is needed to avoid air embolism, such as using CO2 insufflation instead of air insufflation [39,40].
Prototype of a mutibending ultra-slim scope. (A) The distal end has two bending sections for facilitating biliary insertion. (B) Two accessory channels (2.2 and 1 mm) designed to facilitate irrigation during intraductal lithotripsy. (C) Free-hand bile duct insertion of the scope. (Picture courtesy of Prof. Jong H. Moon, MD, PhD, FASGE, FJGES, Director of Digestive Disease Center, SoonChunHyang University School of Medicine, Bucheon/Seoul, Korea).
EXTRACORPOREAL SHOCK-WAVE LITHOTRIPSY
ESWL uses shock waves generated from electrohydraulic or electromagnetic energy. The shock waves are transmitted from outside the body through soft tissue to the target (bile duct stones) under fluoroscopy guidance [41]. The first ESWL for the treatment of bile duct stones was reported in 1986 [42]. Thereafter, difficult stones that could not be removed with a standard ERCP became the most common indication of ESWL for bile duct stones. The overall stone clearance rate is 84.4%–90.2% [43,44]. Post-ESWL complications were reported in 9.1%–15.9% [22,44], and the most common complications were hemobilia (12%) [22] and cardiac arrhythmia (5.9%) [44]. ESWL has several limitations. First, a nasobiliary tube or a T-tube is required to opacify the stone because most of the stones are radiolucent. Second, several sessions are needed to achieve a high stone clearance rate; for example, three sessions are required to achieve a stone clearance rate of 74%. Third, epidural or general anesthesia is necessary during ESWL [43,44]. A randomized study demonstrated that ESWL was inferior to intraductal LL in terms of complete stone clearance (73% vs. 97%, p<0.05), mean number of treatment sessions (3 vs. 1.2, p<0.001), and mean duration of treatment (3.9 days vs. 0.9 days, p<0.001) [45]. The ESGE recommends ESWL when conventional lithotripsy fails and cholangioscopy-guided lithotripsy is not available [4].
BILIARY STENT PLACEMENT
Placement of a temporary biliary plastic stent after ERCP is indicated when stone clearance is not achieved, to avoid stone impaction and prevent cholangitis and pancreatitis [4,46]. In addition, it can decrease the stone size by causing friction between the stent and the stone, which can enhance the success rate of the subsequent ERCP [47,48]. However, ERCP should be repeated within 3–6 months to avoid cholangitis [4,47]. A long-term stent should be reserved for high-risk patients with a short life expectancy owing to the risk of recurrent cholangitis [46]. The additional use of choleretic agents (i.e., ursodeoxycholic acid and terpene combination) showed no benefit on stone size reduction or stone clearance in a prospective study in 51 patients by Lee et al. [49]. After a fully covered self-expandable metal stent (FCSEMS) was placed in patients with incomplete stone clearance, the subsequent ERCP achieved complete stone clearance in 82%–83%. The FCSEMS not only provides friction to reduce the size of the stone but also expands the bile duct orifice. However, the risk of stent migration is 9.5%–22% [50,51]. Although the ESGE does not recommend the use of FCSEMS [4], the ASGE [6] states that FCSEMS may facilitate the removal of difficult bile duct stones, but a subsequent stent exchange or removal is required. An in vitro study demonstrated that drug-eluting FCSEMS was able to reduce the stone mass [52]. However, clinical studies on the benefits of drug-eluting FCSEMS are needed before applying this treatment in clinical practice.
CONCLUSIONS
EPLBD, with a balloon diameter that does not exceed the bile duct diameter after a limited sphincterotomy, is recommended as the first step for removing difficult stones where there is no contraindication. If EPLBD fails, either cholangioscopy-guided lithotripsy or ML can be chosen. However, cholangioscopy-guided lithotripsy has a higher success rate than ML. ESWL is an alternative when ML fails and cholangioscopy-guided lithotripsy is not available. Temporary biliary stenting is indicated when every technique has failed, or when the duration of the procedure has become too long but complete stone clearance is still not achieved during that session. An indefinite biliary stent is reserved only for patients with a short life expectancy (Fig. 5).
Notes
Conflicts of Interest: The authors have no potential conflicts of interest.
Funding
This article was funded by a grant for International Research Integration: Chula Research Scholar, Ratchadaphiseksomphot Endowment Fund and Center of Excellence for Innovation and Endoscopy in Gastrointestinal Oncology, Faculty of Medicine, Chulalongkorn University.
Acknowledgements
The authors sincerely thank Prof. Jong H. Moon, MD, PhD, FASGE, FJGES, Director of Digestive Disease Center, SoonChunHyang University School of Medicine, Bucheon/Seoul, Korea, for the image of the multibending ultra-slim scope prototype.