Underestimation of endoscopic size in large gastric epithelial neoplasms
Article information
Abstract
Background/Aims
Endoscopic submucosal dissection (ESD) is an effective method for resecting gastric adenomas and adenocarcinomas. A significant discrepancy was observed between endoscopic and pathological sizes in samples obtained from patients undergoing ESD. This study elucidates the factors affecting size discrepancy after formalin fixation.
Methods
The records of 64 patients with 69 lesions were analyzed, including 50 adenomas and 19 adenocarcinomas. Data on location, gross shape, histology, and size after fixation in formalin were collected.
Results
The mean size of the resected specimen appeared to decrease after formalin fixation (37.5 mm prefixation vs. 35.8 mm postfixation, p<0.05). The mean long axis diameter of the lesions was 20.3±7.9 mm prefixation and 13.4±7.9 mm postfixation. Size differences in lesions smaller than 20 mm were significantly greater than those in lesions larger than 20 mm (7.6±5.6 mm vs. 2.5±5.8 mm, p<0.01). In multivariate analysis, a tumor size of ≥20 mm was found to be an independent factor affecting size postformalin fixation (p<0.05).
Conclusions
The endoscopic size of lesions before ESD may be underestimated in tumors larger than 20 mm in size. Therefore, increased attention must be paid during ESD to avoid instances of incomplete resection.
INTRODUCTION
Endoscopic submucosal dissection (ESD) is the safest and most effective method for treating malignant tumors and precancerous lesions confined to the gastric mucosa.1 The absolute indications for gastric ESD include endoscopic treatment of differentiated intramucosal tumors, elevated lesions (measuring ≤2 cm), depressed lesions (≤1 cm), and no evidence of lymph node metastasis.2 Studies on the probability of lymph node metastasis in malignant gastric tumors were based on the size of the resected lesion measured after formalin fixation. However, a specimen obtained after surgery was fixed in formalin for a certain period of time, which led to size reduction.3-5
Lesion size is an important parameter to consider when avoiding incomplete resection in ESD.6 The larger the size of the early gastric lesion, the greater the possibility of lymph node metastasis and adenoma accompanied by cancer.7 To date, studies on lesion size have compared microscopic size with the size measured during the endoscopic procedure.8,9 The endoscopic lesion size may differ from its actual size because of gastric movements and technical limitations. In this study, we aimed to compare the pre- and postfixation tumor size of gastric adenoma and adenocarcinoma specimens obtained following ESD, and to identify the changes in size depending on lesion characteristics.
METHODS
Selection of participants
Between July 2013 and January 2014, 69 lesions of 64 patients who underwent gastric ESD at a tertiary medical center were investigated. All patients were diagnosed with either gastric adenoma or carcinoma by endoscopic biopsy prior to treatment. Among gastric cancer patients, individuals with absolute and expanded indications for ESD were included. The absolute indications included an elevated (<2 cm) or a depressed (<1 cm) lesion among those with differentiated intramucosal carcinomas without ulcers. The lesions that comprised expanded indications for performing ESD were as follows: differentiated intramucosal carcinomas >2 cm in diameter without ulcers, <3 cm in diameter with ulcers, those with submucosal invasion <500 µm and are <3 cm in diameter, and undifferentiated intramucosal carcinomas with a diameter of <2 cm without ulcers. Patients with early gastric carcinoma and lymph node metastasis, those who did not have any indication for ESD, and those who did not provide consent to participate in the study were excluded.
The length of the lesion in the tissue specimen obtained immediately after endoscopic resection and postformalin fixation was assessed based on the patient characteristics and histological findings. The factors affecting the differences in size were compared and analyzed.
Endoscopic resection
All procedures were performed by four endoscopic specialists with experience in performing more than 100 cases of ESD, using a gastroscope (GIF-Q240 or GIF-Q260; Olympus Optical, Tokyo, Japan). The characteristics of all lesions, such as the site of occurrence, gross findings, presence of ulcers, and erosions, were inspected, and the gross findings were categorized as I, IIa, IIb, IIc, and III according to the Paris endoscopic classification of early gastric cancer.
A 5-mm margin was marked outside the lesion using a snare tip; normal saline was injected into the submucosa surrounding the lesion. An incision was made circumferentially around the lesion using a needle knife (KD-1L-1; Olympus Optical). Submucosal dissection was performed using an IT knife (insulated-tip diathermic knife; KD-610L; Olympus Optical) and an IT knife-2 (KD-611L; Olympus Optical).
Preparation and evaluation of the resected specimen
The tissues obtained following ESD were pinned on a polystyrene plate; the endoscope was then used to check the margin of the lesion and to measure the long axis diameter. When it was difficult to observe the lesion in detail, chromoendoscopy using indigo carmine or narrow-band imaging was performed. One endoscopist evaluated the long and short-axis diameters of the lesions.
The pinned tissue was fixed using formaldehyde, and the microscopic size of the lesions (long- and short-axis diameters) was measured by three pathologists. Resection was classified as complete or incomplete. The degree of differentiation, proportion of undifferentiated carcinomas, and presence of adenomas were evaluated to exclude carcinomas.
Measurement of the results of the procedure
General characteristics, site and gross findings of the lesion, length of whole resected tissue and lesions, size differences between pre- and postformaldehyde specimen fixation, histopathological diagnosis, complete resection rate, and whether carcinoma was composed of adenoma or undifferentiated histology were thoroughly observed. The site of the lesion was divided into the lower and upper halves, based on whether it was located in the antrum and pylorus or in the rest of the areas, respectively.
Gross findings were classified as either ‘elevated’ or ‘others’ if there was a raised appearance (I or IIa type) or a depression (IIc, IIb, or IIa+IIc type), respectively, in agreement with the Paris classification. Depending on the degree of cell and structural atypia, adenomas were diagnosed as low- or high-grade. We classified low-grade adenomas as ‘non-advanced’ tumors, and high-grade adenomas and adenocarcinomas as ‘advanced’ tumors. Lesions with ulceration or erosion were documented as mucosal injuries. The specimens were evaluated for changes in size postformalin fixation based on the various characteristics of the lesions.
Statistical analysis
The Wilcoxon test was used to compare the long axis diameters of the entire resected tissue. Since the “size difference after formalin fixation” is a continuous variable, the independent t-test was used to compare the mean values of both groups if normality was ensured. The median values of the two groups were compared using the Mann-Whitney U-test when normality was not observed. Significant variables in the univariate analysis were entered into the multivariate analysis using binary logistic regression analysis. Goodness-of-fit tests for logistic regression models were performed using the Hosmer-Lemeshow test. Statistical significance was set at p<0.05. All data were analyzed using the IBM SPSS ver. 22.0 (IBM Corp., Armonk, NY, USA).
Ethical statements
The study was conducted prospectively after obtaining approval from Institutional Review Board of Presbyterian Medical Center (IRB No: 2013-06-19), and written informed consent was obtained from all participants.
RESULTS
General characteristics
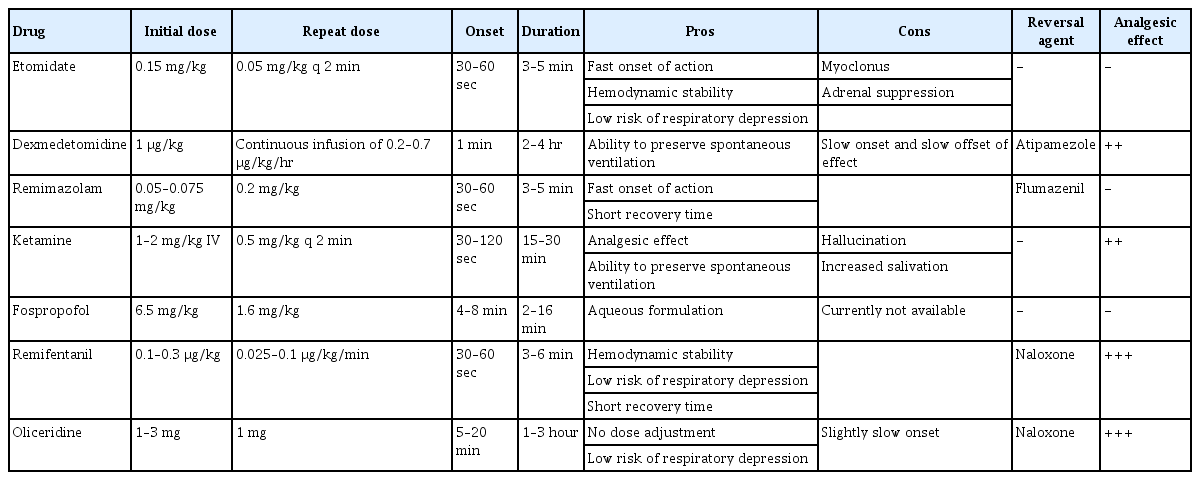
Sixty-nine lesions were analyzed, including 50 adenomas and 19 adenocarcinomas (Table 1). The mean patient age was 66 years. The mean size of the resected tissue was 37.5 mm before formalin fixation and 35.8 mm after fixation; this difference was statistically significant (4.53%, p=0.036). The mean difference in size of the lesions postformalin fixation was 6.8 mm; 7.6 mm and 4.6 mm for the adenomas and adenocarcinomas, respectively. The complete resection rate by ESD was 93% (64 cases); 90% for adenomas and 100% for adenocarcinomas.
Differences in size postfixation
The normality and multivariate normality of the differences in size postfixation were tested, and Mardia’s multivariate kurtosis was 34.963 (z=–0.013, p=0.989), thus satisfying normality. Univariate analysis was performed using the independent t-test, and variables of <0.10 were adjusted and assessed in a multivariate regression analysis. The goodness-of-fit test of the regression model was based on the residual test, and the Kolmogorov-Smirnov normality test with standardized residuals and Breusch-Pagna’s heteroscedasticity test residuals were analyzed.
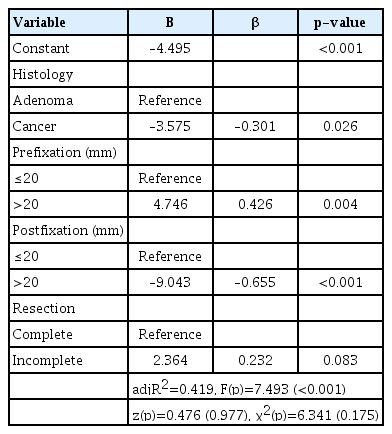
In the univariate analysis using an independent t-test, there was a significant difference between the prefixation (p=0.016) and postfixation (p<0.001) lesion sizes. The difference was 5.6 mm for lesions <20 mm and 2.5 mm for lesions >20 mm postfixation, indicating that larger lesions were associated with smaller differences in size (Table 2).
A binary logistic regression analysis was performed to evaluate the effects of histology, prefixation, postfixation, and resection on the size difference by including those with p<0.10 in univariate analysis. Regression analysis showed that histology (p=0.026), prefixation (p=0.004), and postfixation (p<0.001) had a significant effect on the difference in sizes (Table 3). Carcinomas were associated with less variation in size compared to adenomas (β=–0.301), and changes in size of lesions >20 mm were larger in prefixation (β=0.426) and smaller in postfixation (β=–0.655). The most significant factor that influenced size change was postfixation, with an explanatory power of 41.9%. The goodness-of-fit test of the regression model satisfied the normality of the residuals (p=0.977) and homoscedasticity of the standard residuals (p=0.175).
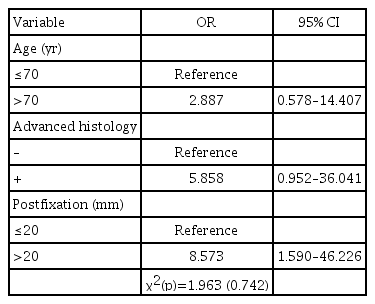
Size increases after formalin fixation
Factors associated with an increase in size were assessed using univariate analyses, including Fisher exact test. The variables that achieved significance (p<0.10) were adjusted, and multivariable analyses were performed using binary logistic regression analyses. The goodness-of-fit test of the logistic regression model was performed using the Hosmer-Lemeshow test. Univariate analysis showed that advanced histology (p=0.040) and postfixation (p=0.007) had a significant effect on the increase in size (Table 4).
Binary logistic regression analysis was performed using variables with p<0.1 comprising age, advanced histology, and postfixation on size change on univariate analysis (Table 5). Postfixation had a significant effect on size changes (p<0.05). Samples with a diameter of >20 mm had 8.573-times higher odds of having changes in size than those with a diameter of <20 mm. Hosmer-Lemeshow’s goodness-of-fit tests revealed that the model was suitable (p=0.742, >0.05).
DISCUSSION
Local recurrence events after endoscopic resection are more likely to occur in patients who have undergone incomplete resection.10,11 Severe intestinal metaplasia of the mucosa often makes it difficult to define lesion borders, thereby leading to incomplete resection.12 Studies on the differences between endoscopic and microscopic size after endoscopic resection of a gastric adenocarcinoma showed that the difference in size was larger in cases of flattened or depressed lesions, large lesions, or poorly differentiated lesions.8,9
Measurement of lesion size using endoscopy reportedly determines the lesions to be smaller than their actual size, whereas measurement using a probe may be more accurate.13,14 Previous reports have compared the microscopic size after ESD with the lesion size measured during endoscopy; this size may differ from the actual size because the stomach continues to move according to the respiratory and heart rate.6,8,11
All studies on the lymph node metastatic potential of gastric malignant tumors include measuring the size of surgically resected tissues.3,12 Gastrointestinal tissues obtained during surgery are reduced in size by 20%–30% after fixation using a formalin solution.3 The present study showed a significant difference in size before and after fixation of the entire resected tissue, albeit <5% in magnitude. Moreover, the lesion size after resection was determined to be larger than the respective microscopic size (20.3 mm vs. 13.4 mm), further suggesting a reduction in lesion size after formalin fixation.
During endoscopic resection, an area at least 5 mm away from the lesion margin was marked, and the outer layer of the marked area was incised. The complete resection rate of ESD is lower for lesions measuring >20 mm than for smaller lesions, because endoscopic surgeons have difficulty in determining the margins of large lesions.6,8,11 Regarding size discrepancies between pre- and postfixation lesions in this study, the change noted in lesions measuring >20 mm was significantly smaller than that in lesions measuring <20 mm (2.5±5.8 mm vs. 7.6±5.6 mm, p<0.01). This result supports the underestimation of the endoscopic size when dealing with larger lesions.
On comparing the size of the lesion measured before formalin fixation with the histological size measured after fixation, a decrease is generally noticed; however, in some patients, the microscopic size of the lesion is larger.8 Endoscopically resected lesions measuring ≥20 mm are usually flat; thus, it is often difficult to determine their margins because the surrounding tissues have severe intestinal metaplasia.15,16 In this study, multivariate analysis showed that lesions measuring >20 mm when measured histologically after fixation were 8.65 times more likely to increase in size postfixation than those measuring <20 mm.
Although surgeons’ experience in performing endoscopic procedures has increased and various ESD knives have been developed, the rate of complete resection using ESD for gastric carcinomas is approximately 90%.15 Yun et al.15 found that the recurrence rate was higher if the resection-free margin was <3 mm during endoscopic resection. Therefore, it is advisable to mark >5 mm away from the visible margin during ESD for lesions measuring >20 mm. During the resection of gastric epithelial tumors, marking and resecting away from the visible lesion margins may reduce local recurrence.
This observational study compared differences in tumor size before and after formalin fixation of gastric adenoma or carcinoma specimens obtained following ESD; however, it comes with a few limitations. First, after endoscopic resection, the lesion size was measured by a single endoscopist and subjectivity was used when it was difficult to distinguish the lesion margins. Second, when the tissue was fixed to a thin plate after ESD, it could not be fixed using constant pressure. Third, this study assessed and analyzed the difference using only the long axis diameter of the tissue, assuming that the lesion had a round shape and that margin misjudgment would have occurred only when considering the long axis of the lesion. Finally, sampling errors cannot be excluded since the number of cases was small. This is an inherent characteristic of a prospective study, because only patients who visited a single hospital were included, and those who did not provide consent were excluded. Therefore, future prospective large-scale multicenter studies are required to determine whether the findings presented here can be generalized.
This is the first prospective study to evaluate differences in sample size pre- and postfixation following ESD. Our results were similar to those of previous studies that used lesion sizes measured during endoscopy. In addition, there was a higher chance of underestimating lesion size in cases of gastric adenomas or adenocarcinomas measuring ≥20 mm before ESD. The endoscopic resection of such lesions could result in higher rates of incomplete resection, thereby necessitating careful attention.
Notes
Conflicts of Interest
The authors have no potential conflicts of interest.
Funding
None.
Acknowledgements
I would like to express my sincere gratitude to all the doctors and nurses of the Gastrointestinal Endoscopy Center in the Presbyterian Medical Center, Jeonju, Korea.
Author Contributions
Conceptualization: JSS, MAY, YJL, JWC; Data curation: JSS, BSK, MAY, JWK; Formal analysis: YJL, GMJ, JWK; Investigation: JSS, BSK, MAY, GMJ; Methodology: JSS, BSK, MAY, YJL; Project administration: GMJ, JWK; Resources: JSS, MAY, YJL, JWC; Software: YJL, GMJ, JWK; Supervision: JWC; Validation: YJL, JWK; Visualization: MAY, GMJ; Writing–original draft: JSS, JWC; Writing–review & editing: all authors.