Peroral endoscopic myotomy versus Heller’s myotomy for achalasia hospitalizations in the United States: what does the future hold?
Article information
Achalasia is a rare neurodegenerative motility disorder of the esophagus characterized by ineffective lower esophageal sphincter relaxation and the absence of organized peristalsis leading to dysphagia.1 First described in the early 1990s, Heller’s myotomy (HM) is the gold standard treatment of choice for achalasia.2 However, peroral endoscopic myotomy (POEM), a minimally invasive endoscopic technique, has gained immense popularity for the management of achalasia since its inception in Japan in 2008.3 It has also been widely endorsed by the American Society for Gastrointestinal Endoscopy in clinical practice.3 Although numerous studies have been performed to compare the efficacy and safety of POEM and HM, there continues to be a significant paucity of data for achalasia hospitalizations that undergo either POEM or HM at a national level.
We analyzed the National Inpatient Sample to identify all adult (≥18 years) achalasia patients admitted to the hospital after POEM or HM in the United States from 2016 to 2019. Hospitalization characteristics and clinical outcomes were compared between the POEM and HM cohorts. SAS ver. 9.4 (SAS Institute, Cary, NC, USA) was used for statistical analysis and p-values ≤0.05 were considered statistically significant.
A total of 1,885 and 11,150 achalasia patients were admitted to the hospital after POEM and HM, respectively, primarily at large urban teaching hospitals (Table 1). We did not find a statistically significant difference in the mean age between the POEM and HM cohorts (57.6 vs. 56.7 years, p=0.14). A significant Caucasian predominance was noted in both subgroups. Although achalasia hospitalizations that underwent POEM and were admitted to the hospital after had a higher comorbidity burden, we did not find a statistical difference in the mean length of stay (3.7 vs. 3.4 days, p=0.36) and mean total healthcare charge ($66,151 vs. $65,468, p=0.77) between the two groups. Furthermore, inpatient mortality was not observed in the POEM cohort. However, the all-cause inpatient mortality rate in the HM cohort was 0.002% (30 patients) (Table 1).
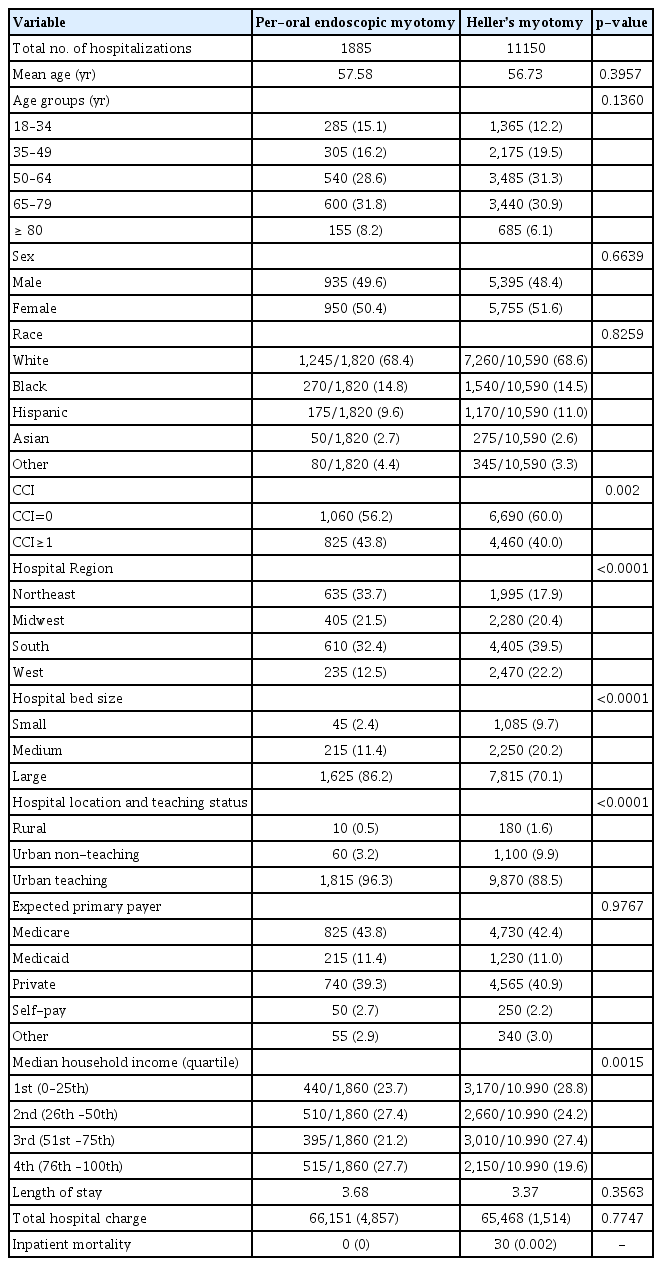
Comparative analysis of hospitalization characteristics and clinical outcomes for peroral endoscopic myotomy and Heller’s myotomy for achalasia hospitalizations in the United States from 2016 to 2019
Our data reflect an overall excellent safety profile and similar recovery times and costs associated with POEM and the gold standard procedure for the management of achalasia, HM. However, even though patients who underwent POEM had a higher comorbidity burden, the all-cause inpatient mortality in the POEM cohort was 0% compared to 0.002% (30 patients) in the HM cohort. Hence, POEM may be a less invasive and safer alternative for the management of achalasia in patients with more comorbidities. Further prospective multicenter studies are needed to investigate these findings.
Notes
Conflicts of Interest
The authors have no potential conflicts of interest.
Funding
None.
Author Contributions
Conceptualization: DSD, SI, MRS, MAH; Data curation: DSD, CIC; Formal analysis: CIC; Investigation: all authors; Methodology: all authors; Project administration: all authors; Resources: DSD, CIC; Software: CIC; Supervision: DSD, MAH; Validation: all authors; Visualization: all authors; Writing–original draft: all authors; Writing–review & editing: all authors.
