Risk Factors for Prolonged Hospital Stay after Endoscopy
Article information
Abstract
Background/Aims
The recovery room used after endoscopy has limited capacity, and an efficient flow of the endoscopy unit is desired. We investigated the duration of hospital stay after endoscopy and the risk factors for prolonged hospital stay among outpatients.
Methods
We retrospectively studied consecutive patients who underwent esophagogastroduodenoscopy or colonoscopy at the Toyoshima Endoscopy Clinic. We collected data on age, sex, body weight, midazolam and pethidine dosage, respiratory depression during endoscopy, and duration of hospital stay after endoscopy (scope out to check out). Risk factors for prolonged hospital stay (>100 minutes) were identified using multiple logistic regression analysis.
Results
We enrolled 3,898 patients, including 3,517 (90.2%) patients tested under sedation and 381 (9.8%) patients tested without sedation. Overall, 442 (11.3%) patients had prolonged stay (>100 min). The mean time difference between sedation group and non-sedation group was 44.2 minutes for esophagogastroduodenoscopy and 39.1 minutes for colonoscopy. Age (odds ratio [OR], 1.025; 95% confidence interval [CI], 1.014−1.036), female sex (OR, 1.657; 95% CI, 1.220−2.249), and midazolam dose (OR, 1.019; 95% CI, 1.013−1.026) were independently associated with prolonged hospital stay after esophagogastroduodenoscopy, with similar results for colonoscopy.
Conclusions
Old age, female sex, and midazolam dose were independent risk factors for prolonged hospital stay after endoscopy.
INTRODUCTION
Endoscopic sedation reduces distress during invasive procedures; however, esophagogastroduodenoscopy (EGD) and colonoscopy can be performed without sedation [1-3]. Non-sedated endoscopy offers several potential advantages, such as lower cost, higher efficiency, and decreased post-endoscopic impairment, which allows patients to drive sooner [4]. Small-diameter endoscopes (<6 mm) can improve the tolerability of EGDs when a sedative is not used. On the other hand, the American Society for Gastrointestinal Endoscopy (ASGE) recommends that a combination of an opiate and benzodiazepine is a safe and effective regimen for achieving minimal-to-moderate sedation for EGDs and colonoscopies in patients without risk factors for sedation-related adverse events [5]. In the United States, more than 98% of endoscopists use sedation during EGDs and colonoscopies [6].
Endoscopic sedation requires the use of a recovery room. When space is limited in the recovery room, the relatively longer residual effects of opiate and benzodiazepine administration could be problematic. If there are any delays in the recovery or discharge of patients, endoscopic procedures might have to be paused until the recovery room becomes available. Continued pressure on endoscopy units to improve efficiency, increased demand for endoscopic procedures, and a high patient turnover have led to growing interest in sedation alternatives, such as propofol [7]. Propofol is a short-acting agent with rapid recovery and can promote the general flow of the endoscopy unit [8]. However, propofol manufacturers in Japan and several other countries restrict its use to personnel trained in general anesthesia [9]. Therefore, many facilities use benzodiazepines and/or opiates for endoscopic sedation [10-12]. Our endoscopy-specialized clinic also uses midazolam and/or pethidine [13]. Even when antagonists such as flumazenil and naloxone are used, recovery from sedation takes time. The recovery room is limited in terms of space and time [14], and the endoscopy clinic needs an efficient flow of patients. In this study, we investigated the duration of hospital stay after endoscopy and identified the risk factors for prolonged hospital stay in outpatients.
MATERIALS AND METHODS
Ethics
This retrospective study was approved by the Certificated Review Board of Hattori Clinic on September 4, 2020 (approval no. S2009-U04). Written informed consent was obtained from the study participants [15]. This study was conducted according to the ethical guidelines of the Declaration of Helsinki.
Subjects
We retrospectively reviewed 4,602 consecutive patients who underwent EGD or colonoscopy at the Toyoshima Endoscopy Clinic, an outpatient clinic specialized in endoscopy, between August 16, 2019, and June 1, 2020. The indications for EGD or colonoscopy were symptoms, such as abdominal pain and gastrointestinal bleeding, positive fecal occult blood test, surveillance of polyps in atrophic gastritis, screening for cancer, or physical checkup. The following demographic and clinical characteristics were collected from medical records: age, sex, body weight, doses of midazolam and pethidine, occurrence of respiratory depression during the endoscopy, and duration of hospital stay after endoscopy (scope out to check out). Respiratory depression was defined as a reduction in percutaneous oxygen saturation (<90%) during endoscopy.
Endoscopic examination
Colonic preparation before colonoscopy was performed with 2 L of polyethylene glycol solution. Polyethylene glycol solution or magnesium citrate was added when the stool was not a clear liquid [16].
Experienced endoscopists performed EGD or colonoscopy. Before EGD, local anesthesia of the pharynx was induced using a viscous solution of 2% lidocaine hydrochloride (Xylocaine® Viscous 2%; AstraZeneca Inc., OSAKA, Japan) [17]. For endoscopic sedation, midazolam and/or pethidine were used according to the patient’s response [18]. The doses of midazolam and/or pethidine were determined by each endoscopist. CO2 was used as insufflation agent for all patients, except those with chronic respiratory failure [19]. Flumazenil and/or naloxone were used as antagonists of midazolam and/or pethidine for sedation recovery.
The patients were transferred to the recovery room after the procedure. When Aldrete’s scoring system was 9 out of 10, or more, they were discharged from the recovery room [20]. Their check out time was recorded after they had finished changing their clothes.
Statistical analysis
We compared clinical characteristics between the no sedation group and sedation group using the Welch’s t-test or chi-square test.
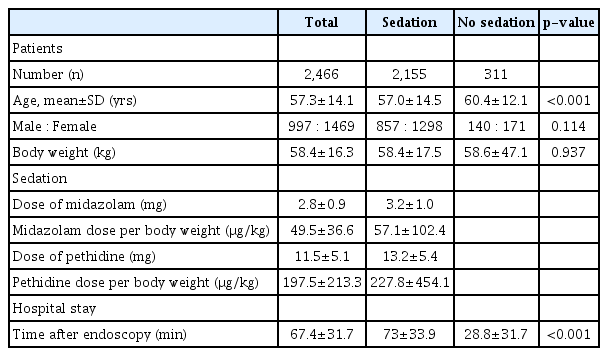
Risk factors for prolonged hospital stay (>100 min) were assessed using multiple logistic regression analysis. Age and dose of each drug were included as continuous variables in the multivariate logistic regression model. Prolonged hospital stay was defined as >100 min. The mean duration of hospital stay after EGD was 67.4±31.7 min (Table 1). In the statistical normal distribution, the mean within 1 standard deviation (SD) includes 68% of the patients, and that within 2 SD includes 95% of the patients. We set the cutoff at 100 min because it is important to predict cases beyond 1 SD. Statistical significance was set at p<0.05. The data were analyzed using Stat Mate IV software (ATOMS, Tokyo, Japan).
RESULTS
During the study period, 4,602 consecutive patients who underwent EGD or colonoscopy were enrolled. We excluded 659 patients with no data for body weight, and 45 patients without data on length of clinical stay after endoscopy. Finally, we included 2,466 patients who underwent EGD and 1,432 patients who underwent colonoscopy.
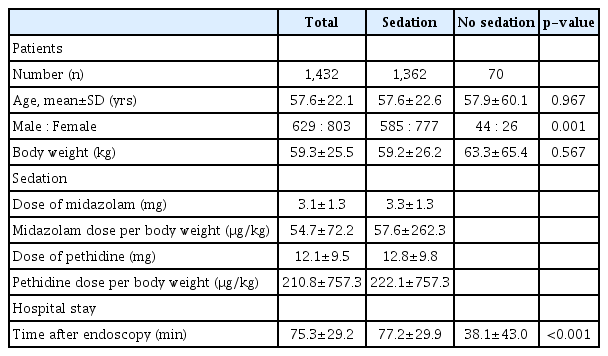
The characteristics of the sedation and no sedation groups after EGD are shown in Table 1. The duration of hospital stay after EGD in the sedation group was significantly longer than that in the no sedation group (73.0±33.9 min vs. 28.8±31.7 min, p<0.001). The mean difference was 44.2 minutes for EGD. The characteristics of the sedation and no sedation groups during colonoscopy are shown in Table 2. The duration of hospital stay after colonoscopy in the sedation group was significantly longer than that in the no sedation group (77.2±29.9 min vs. 38.1±43.0 min, p<0.001). The mean difference was 39.1 minutes for colonoscopy.
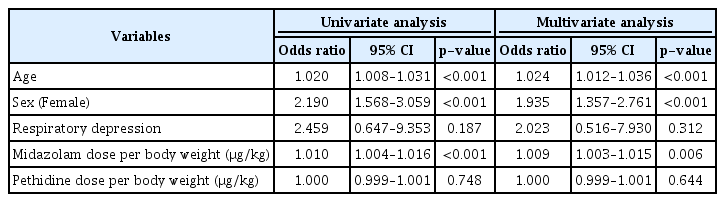
Table 3 shows the results of multivariate analyses of prolonged hospital stay (>100 min) after EGD. A total of 251 patients in the EGD group had a prolonged hospital stay. Age (odds ratio [OR] =1.025; p<0.001), female sex (OR=1.657; p<0.001), and midazolam dose (OR=1.019; p<0.001) were independently associated with a prolonged hospital stay in the EGD group. When these multivariate analyses were performed for the patients who underwent sedation, the results did not change.
Table 4 shows the results of multivariate analyses of prolonged hospital stay (>100 min) during colonoscopy. A total of 191 patients in the colonoscopy group had a prolonged hospital stay. Age (OR=1.024; p<0.001), female sex (OR=1.935; p<0.001), and midazolam dose (OR=1.009; p=0.006) were independently associated with prolonged hospital stay in the colonoscopy group. When these multivariate analyses were performed for patients who underwent sedation, the results were similar. Although the statistical significance disappeared for midazolam dose, the p-value was 0.059. The results of the multivariate analyses did not change, even if the cutoff of prolonged stay was 90 min.
DISCUSSION
We found that the mean time difference between sedated endoscopy and non-seated endoscopy was 44.2 min after EGD and 39.1 min after colonoscopy, and the risk factors for prolonged hospital stay after endoscopy included old age, female sex, and high dose of midazolam.
The ASGE guidelines on sedation during gastrointestinal endoscopy recommend endoscopic sedation because it relieves patient anxiety and discomfort, and improves the outcome of the procedure [5]. However, the disadvantages of sedation include extended hospital stay and increased frequency of adverse events, such as nausea and headache. This study showed that length of hospital stay was extended by 40 min. Informed consent should include information about extended hospital stay.
Recovery in elderly patients is more likely to be slow after endoscopic sedation [21,22], leading to prolonged hospital stay. Female sex was also an independent risk factor for delay. Female sex was reported to be associated with nausea after endoscopy using pethidine [23], and post-endoscopic nausea might affect the delay.
The novel coronavirus disease (COVID-19) has been declared a pandemic by the World Health Organization (WHO) [24,25]. During the COVID-19 pandemic, the WHO issued an advisory to avoid crowded places [26]. The Japanese government also recommended avoiding the three C’s: closed spaces, crowded places, and close contact settings. Endoscopy units could increase the risk of infection from potential airborne droplets and fecal-oral transmission [27,28]. Crowding of the endoscopy unit should be avoided [29]. Minimizing the dose of midazolam or omitting sedation might alleviate congestion, especially among elderly patients.
On the other hand, the Japanese government is promoting a work style reform, advocating for a reduction of overtime hours and avoidance of long working hours [30,31]. Endoscopic clinics or units should consider reducing working hours and increasing productivity. The measures against overtime would include avoiding scheduling elderly patients and patients who desire deep sedation for procedures in the evening and minimizing the dose of midazolam in patients who undergo the procedure in the evening.
Fredman et al. concluded that intravenous administration of the premedicant midazolam (0.5 mg or 2 mg) did not adversely affect early recovery or postoperative cognitive function [32]. In their study, midazolam was used as a premedication before administration of standard general anesthesia, and the dose of midazolam was relatively lower than that used in this study. In our study, the doses of midazolam were 3.2±1.0 mg. The results may change depending on the administration timing and dose.
The limitations of this study include its retrospective design. This study was conducted at a single institution. Nevertheless, the recording of medical data was well controlled. The recovery time might be faster when the patients’ average alcohol intake is high, since it has been reported that alcohol consumption may reduce midazolam bioavailability [33]. However, we could not analyze the impact of alcohol consumption in this study. Our multivariate logistic regression analysis used age as continuous variables, and showed no specific age as risk factor. A follow-up prospective study should be performed to confirm and clarify the characteristics of patients with prolonged hospital stay after endoscopy.
In conclusion, hospital stay due to endoscopic sedation was prolonged by about 40 minutes when using midazolam and/or pethidine. Old age, female sex, and midazolam dose were independent risk factors for prolonged hospital stay after endoscopy.
Notes
Conflicts of Interest: The authors have no potential conflicts of interest.
Funding
None.
Author Contributions
Conceptualization: Osamu Toyoshima
Data curation: Tatsuya Matsuno, Masataka Irokawa, Toru Arano
Formal analysis: Toshihiro Nishizawa
Investigation: Shuntaro Yoshida
Resources: OT
Writing-original draft: TN
Supervision: Takanori Kanai, Kazuhiko Koike
Writing-review&editing: Hirotoshi Ebinuma, Hidekazu Suzuki