INTRODUCTION
Endoscopic retrograde cholangiopancreatography (ERCP) is a widely performed procedure for diagnosing and treating pancreaticobiliary disease. During ERCP-related procedures, selective biliary cannulation is an elementary and first-step technique for subsequent procedures such as stone removal and stenting. However, it is not always possible to accomplish standard biliary cannulation through the orifice of the major papilla; transpapillary biliary cannulation has been reported to fail in 5% to 15% of cases despite recent improvements in ERCP methods.1-4 Post-ERCP pancreatitis (PEP) is the most common and serious complication associated with the procedure, occurring at an incidence of 2% to 10%. Frequent attempts at papilla cannulation and precutting are the main risk factors for PEP.5-12 Precutting is an alternative technique for accessing the common bile duct (CBD) when standard biliary cannulation is not possible. Being a reported risk factor for PEP and other adverse events, cannulation using this method is considered a last resort by expert endoscopists. It has recently been postulated that early transition from standard transpapillary cannulation to a precutting technique can reduce the incidence of PEP13-15 since the repeated failed attempts at cannulation (before switching to precutting) may be primarily involved in PEP onset. Needle-knife fistulotomy (NKF), one of the precutting methods of making an incision from the papilla roof without touching the orifice, performed as an initial procedure for biliary access, has reduced the risk of complicating PEP.16-19 Hence, a primary or early precutting strategy may be effective for preventing PEP, but the safety and efficacy of these approaches have not been fully elucidated.
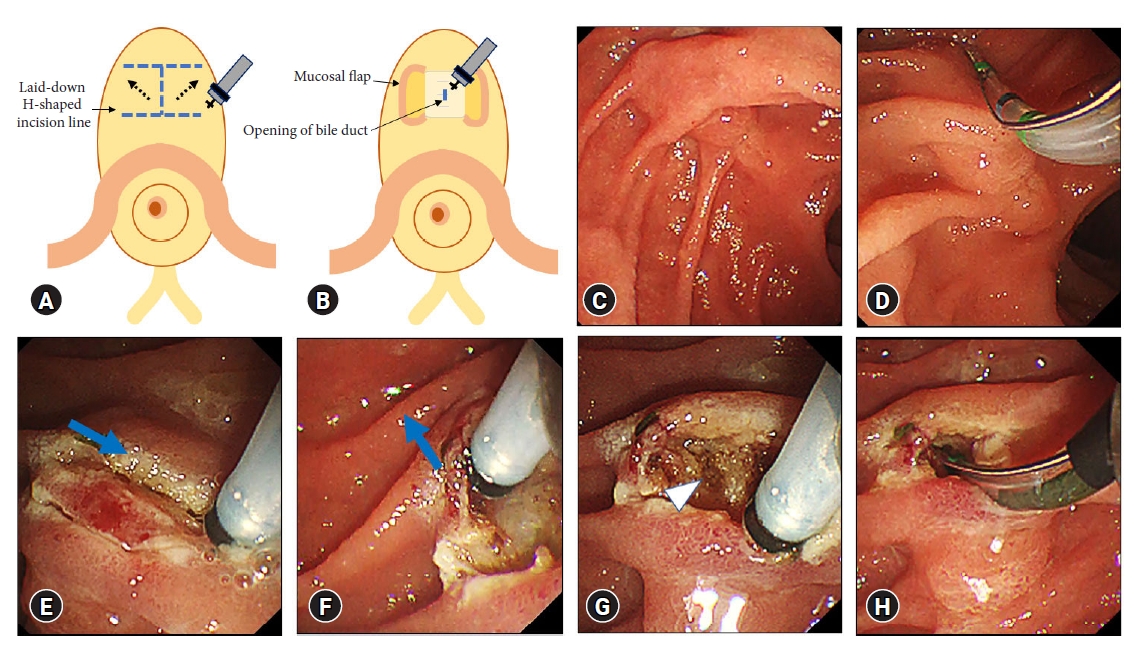
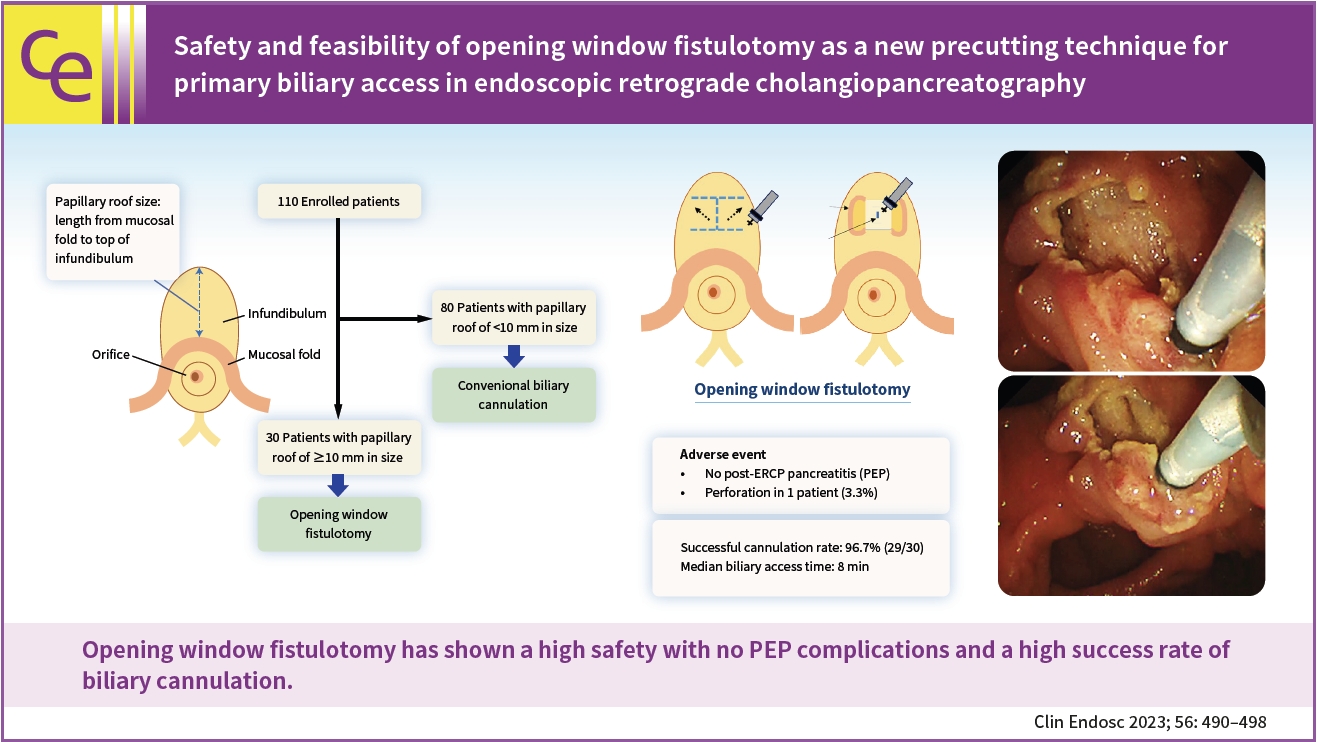
Transpapillary cannulation in patients with a large and extended infundibulum is empirically challenging. For such cases, we have recently tested a unique NKF method, termed opening window fistulotomy, as a primary procedure for biliary access in which a suprapapillary laid-down H-shaped incision is made without touching the orifice. This technique allows for detailed observation of the duodenal submucosa in a wider field of view owing to the large incision surface, enabling a suprapapillary incision at an appropriate site to open the bile duct ostium.
Herein, we aimed to prospectively clarify the safety and feasibility of our unique precutting method, i.e., NKF with the opening window method, as an initial procedure for biliary cannulation.
METHODS
Patients
Patients aged Ōēź20 years who underwent ERCP to treat biliary tract disease were included in this study. Patients were excluded from the analysis according to the following criteria: previous sphincterotomy, prior gastric surgery such as Billroth II and Roux-en-Y reconstruction, duodenal stenosis, ampullary cancer, the requirement of a pancreatogram, and refusal or inability to provide informed consent. In addition, patients needing urgent ERCP-related procedures, such as acute cholangitis, and those deemed unsuitable for participation in this study due to their general condition were also excluded.
The primary outcome of this investigation was to evaluate the incidence of ERCP-related complications, especially PEP, in patients who underwent opening window fistulotomy as the primary means of biliary access. The secondary outcome was to assess the success rate of biliary cannulation using the new technique. The time from the initial attempt at biliary cannulation or the start of precutting until successful biliary access was recorded for each patient. ERCP-related adverse events were defined according to consensus criteria.20 PEP was defined as an elevation in serum amylase level at least three times the normal level on the day following ERCP accompanied by new-onset abdominal pain. Asymptomatic hyperamylasemia was defined as an increase in serum amylase level at least three times the normal level, without abdominal pain. Bleeding was identified using clinical signs such as hematemesis, melena, a decrease in hemoglobin concentration of more than 2 g/dL, and continuous blood oozing during the ERCP procedure requiring hemostasis. Perforation was recorded as the detection of luminal contents outside the duodenum or leakage of contrast or retroperitoneal air during the procedure. Cholangitis was diagnosed based on clinical evidence of infection (fever, leukocytosis, or abdominal pain) in patients with elevated serum biochemical liver test results.
This study primarily evaluated the safety of opening window fistulotomies. The sample size was set to 30 by applying the stopping rule, which was determined by considering the number of cases that could be registered at our institution. First, five patients were registered in this study and received the new technique. The trial was terminated when severe adverse events occurred in two or more cases. Next, five patients were included to bring the total study number to ten. Similarly, the trial was discontinued if two or more of the ten cases were complicated with severe adverse events. Thereafter, if the number of severe adverse events was one or fewer of the ten cases, an additional 20 cases were registered in the study.
ERCP procedures
In the prone position, the patients underwent ERCP using a standard duodenoscope (TJF-260V or TJF-Q290V; Olympus Optical Co., Ltd.). Before ERCP commencement, patients were administered intravenous midazolam and pethidine for sedation and intravenous hyoscine butyl bromide for duodenal relaxation. Routine prophylactic administration of a non-steroidal anti-inflammatory drug suppository for PEP prevention was not performed in this study. Carbon dioxide insufflation is regularly performed during ERCP.
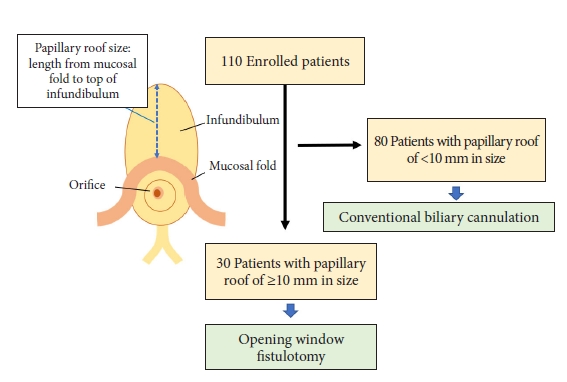
We carefully evaluated the major papilla by assessing the length of the papillary roof from the mucosal fold to the top edge of the infundibulum using a catheter. If the papillary roof length was Ōēź10 mm, opening window fistulotomy was performed as the initial procedure for biliary access using a needle-knife papillotome (Splash M knife; Pentax). A VIO 300D (ERBE Elektromedizin) was employed as the electrical cutting generator in ENDO CUT I mode, effect 2, cut duration 2, cut interval 2, and 60 W. Standard wire-assisted biliary cannulation was performed if the length of the papillary roof was <10 mm. CBD cannulation was performed using a sphincterotome (Correctome; Boston Scientific) or triple-lumen cannula (Tandem, Boston Scientific) preloaded with a hydrophilic guidewire (M-through; Asahi Intecc).
Biliary access using the unique precutting technique, termed opening window fistulotomy, was evaluated for feasibility (Fig. 1, Supplementary Video 1). Initially, two parallel incisions were made in the infundibulum perpendicular to the axis of the major duodenal papilla while avoiding contact with the orifice. Subsequently, an incision along the axis of the papilla was created to connect the two parallel incisions, and a laid-down H-shaped incision line was made. After these initial cuttings, the incision surface was opened like a window by elevating the right and left mucosal flaps. The submucosa and sphincter of Oddi were observed in a wider field of view because of the large incision surface, thus allowing a suprapapillary incision at an appropriate site to open the bile duct ostium. An additional incision along the axis of the papilla was slowly made and stopped when bile juice or pinkish or whitish bile duct mucosa was visible. Afterward, selective biliary cannulation through the fistula was performed using the wire-guided technique. After successful biliary cannulation, extended endoscopic sphincterotomy or endoscopic papillary balloon dilation through the fistulotomy site was performed according to the respective ERCP-related procedures such as stone removal and stenting.
After the procedure, the patients were observed carefully with close attention to the appearance of abdominal symptoms. Laboratory examinations were performed the following day to check for procedure-related complications. When abdominal symptoms or abnormal laboratory findings were found, inspection by computed tomography or ultrasonography, along with appropriate treatment, was performed.
Statistical analysis
For clinicodemographic patient characteristics, categorical variables were expressed as numbers and percentages, whereas continuous variables were expressed as medians and ranges.
Ethical statements
This prospective study was conducted between December 2017 and October 2020 at the Aichi Cancer Center Hospital to evaluate the safety and feasibility of opening window fistulotomy. The study adhered to the current ethical guidelines of the Declaration of Helsinki and was conducted following the requirements of the Institutional Review Board of the Aichi Cancer Center (approval number: 2017-1-132). Written informed consent was obtained from all participants. This study was registered with the University Hospital Medical Information Network Clinical Trial Registry (ID 000030511).
RESULTS
Baseline patient characteristics
A total of 110 consecutive patients were enrolled in this prospective study until the number of cases of opening window fistulotomy reached 30. The baseline characteristics of the enrolled patients are summarized in Table 1. Of the 110 patients, 57 were male (51.8%), and 53 were female (48.2%). The median age of the patients was 69 years (range, 30ŌĆō86 years). The median papillary roof size, i.e., the length from the mucosal fold to the top of the infundibulum, was 6 mm (range, 3ŌĆō20 mm). Patients with a papillary roof size Ōēź10 mm and <10 mm were numbered 30 and 80, respectively (Fig. 2). Accordingly, 27% of the 110 patients underwent opening window fistulotomy for primary biliary access. Figure 3 presents representative endoscopic images of the procedure, showing the submucosa and sphincter of the papilla in a wider field of view. Of these, 13 were men (43.3%), and 17 were women (56.7%). The median patient age was 70 years (range, 38-85 years), and the median papillary size was 13 mm (range, 10ŌĆō20 mm). Antiplatelet or anticoagulant medications were administered to four patients, all of whom temporarily discontinued their regimens for the procedure. The indications for ERCP in the opening window fistulotomy cases were choledocholithiasis (n=9), malignant stenosis (n=19), and sclerosing cholangitis (n=2). Opening window fistulotomy could be performed in all patients with a papillary roof size Ōēź10 mm enrolled in this study. No patient had conditions rendering the procedure impossible, such as papilla inside the duodenal diverticulum and massive tumor invasion into the papilla.
ERCP-related complications
No patient experienced PEP in the fistulotomy cases (Table 2), and asymptomatic hyperamylasemia was not observed. None of the patients exhibited bleeding, cholecystitis, or cholangitis after ERCP. A small amount of bleeding from the incision surface was observed in three patients during NKF. Since the hemorrhage stopped immediately and spontaneously without hemostasis and did not interfere with the ensuing incision or biliary cannulation, these cases were not considered complications according to the above-described criteria. Retroperitoneal duodenal perforation was observed on fluoroscopy in one (3.3%) patient with malignant biliary stenosis, which did not occur during the fistulotomy but rather during the insertion of a procedure device after successful biliary cannulation. A metallic stent was inserted across the papilla for biliary drainage to prevent bile leakage during the same ERCP session. After the procedure, the patient had no abdominal pain, fever, or other signs of peritoneal irritation and was managed conservatively without surgical intervention.
ERCP-related procedures
The ERCP-related procedures used in this study are presented in Table 3. In fistulotomy cases, endoscopic sphincterotomy and endoscopic papillary balloon dilation through the fistulotomy site were performed in 22 (73.3%) and 3 (10.0%) patients, respectively, without any detectable adverse events related to the treatments. Endoscopic biliary stenting was performed in 17 (56.7%) patients, with plastic stents in six patients (20.0%) and metallic stents in 11 patients (36.7%). Peroral cholangioscopy was performed in four patients (13.3%). None of the patients underwent unintended pancreatic duct cannulation or subsequent prophylactic pancreatic stenting.
The rate of successful biliary cannulation was 96.7% (29/30 patients). The median duration of biliary cannulation was eight minutes (range, 3ŌĆō15 minutes). One patient with obstructive jaundice caused by a gastric cancer with liver metastatic lesion did not achieve biliary access using opening window fistulotomy. Although the fistulotomy method was conducted in the prescribed manner, CBD opening could not be found. During the same session, successful biliary cannulation was performed using an endoscopic ultrasound-guided rendezvous technique. All remaining patients achieved successful biliary access through opening window fistulotomy and underwent their respective ERCP-related procedures through the fistula.
DISCUSSION
In the current study, we prospectively evaluated the safety and feasibility of our unique NKF technique, termed opening window fistulotomy, as a primary procedure for biliary access in patients with a long papillary roof Ōēź10 mm. No PEP was recorded, and the technique was successful in virtually all cases. This precutting technique may represent a safe and effective option for providing operators with a wider field of view for biliary access.
Selective biliary cannulation through the major papilla is an essential and prerequisite step in ERCP-related operations; however, it is also the largest hurdle in successfully performing the desired treatment. Without initial biliary access, almost all subsequent ERCP-related procedures are impossible. As the first step, biliary cannulation is one of the procedures most related to adverse events, especially PEP. PEP is a frequent and problematic complication of ERCP-related treatments and is sometimes severe and potentially fatal.
Precutting is a biliary access technique used to overcome difficulties in cannulating the CBD. Various methods for precutting have been reported, including transpancreatic precutting, papillotomy, NKF, and needle-knife precutting over the pancreatic stent.2 Of these precutting methods, NKF was conducted and evaluated in this study. In standard NKF, an incision is made along the axis of the papilla oriented at the 11 to 12 oŌĆÖclock position on the infundibulum. In our NKF method, a wider incision surface can be obtained by adding vertical incisions to the papilla axis. This technique facilitates the observation of the submucosa and sphincter of the papilla by a wider field of view compared with standard NKF, thus providing safer and more reliable access to the CBD. Since opening book fistulotomy enables clear identification of the incision point for biliary access owing to a large incision surface, it may be positioned as a rescue technique when the appropriate incision site to open the bile duct ostium is unknown or uncertain with standard NKF. However, there are concerns regarding the risk of bleeding and perforation due to the additional transverse incisions. In several cases, bleeding from the incision surface was observed during NKF, but these were self-limiting, resolved spontaneously, and did not interfere with the procedure. No patient with bleeding required hemostasis during or after the operation. Similarly, none of the patients suffered perforation caused by the NKF itself, although one case was complicated by perforation during the insertion of another device. In addition, since our NKF method required extra incisions in the papilla to obtain a wide incision surface, there was a disadvantage that patients with a small papillary roof could not be included in this technique. Accordingly, opening window fistulotomy was performed only in patients with a papilla Ōēź10 mm, which accounted for approximately a quarter (27%) of cases.
Precutting has been previously reported to be associated with postoperative PEP onset. However, multiple failed attempts at biliary cannulation and repeated pancreatic duct access have also been found to increase the risk of PEP.5-12 Since precutting is positioned as a rescue technique for biliary access and is usually performed after repeated cannulation attempt failures, it is difficult to determine whether the PEP risk is primarily increased by precutting, multiple attempts at cannulation or both. Recently, early transition from standard transpapillary cannulation to precutting was reported to be effective in reducing PEP.13-15 In addition, primary precutting without attempting standard cannulation is useful in preventing PEP.16-19 In a single-arm prospective study, 55 patients with one or more risk factors for PEP received NKF as the initial treatment of biliary cannulation.18 None of the patients experienced PEP, and the CBD cannulation success rate was 96.4% (53/55 patients). In a randomized control study of 207 patients, the biliary cannulation success rate and the incidence of adverse events were compared between NKF and conventional cannulation methods as primary biliary access.17 PEP was significantly less frequent in the NKF group than in the conventional cannulation group (0% vs. 9.2%, p<0.001), and the successful cannulation rate was higher in the NKF group (97.9% vs. 89.7%, p=0.005). In contrast, the total mean cannulation time was longer in the NKF group (257 vs. 171 seconds, p=0.004). In the present study, the successful cannulation rate of patients undergoing NKF with the opening window method was 96.7% (29/30 patients), which is comparable to previous reports. However, the median duration for biliary access was 8 minutes, slightly longer than that of previously described techniques. Our method's time for biliary access was presumably longer, as it required a more extensive incision process than the standard NKF. In agreement with earlier studies, none of the patients had PEP complications. In primary NKF, a suprapapillary incision without touching the orifice and subsequent procedures through the fistulotomy site may minimize mechanical and thermal injury to the ampulla and pancreatic duct. No patient received unintended pancreatic duct cannulation, thus mitigating the risk of PEP. Therefore, NKF for primary biliary access may be effective, particularly in patients at a high risk of PEP. Female patients aged <60 years with non-dilated CBD, sphincter of Oddi dysfunction, or a history of pancreatitis are reportedly at high risk of PEP, with an incidence as high as 37%;7,9,12,21,22 hence, to prevent PEP development, patients belonging to this category are suggested to undergo NKF for primary biliary access. Difficulty in biliary cannulation is also associated with PEP development,7 and transpapillary cannulation in patients with large papillary roofs is empirically challenging. As in the strategy of the current study, patients with a large papillary roof were considered suitable candidates for our technique.
This study has several limitations. Firstly, the study design consisted of a single arm. The 110 enrolled patients were divided into a primary fistulotomy group and a standard biliary cannulation group according to the length of the papillary roof. However, comparative evaluations could not be performed between the groups regarding complication incidence and biliary cannulation success rates. Biliary access through the papilla with a large and extended infundibulum is difficult; therefore, such procedures have a higher incidence of PEP and reduced successful cannulation rate. However, none of the patients receiving NKF experienced PEP, and the successful cannulation rate was comparatively high, suggesting that our biliary access strategy using the opening window fistulotomy technique was safe and feasible. Second, because this study contained a limited sample obtained from a single cancer center, the generalizability of our results is limited. The primary purpose of the current investigation was to evaluate the safety of NKF with opening window fistulotomy, especially with regard to PEP, as preliminary research. A subsequent multicenter, randomized controlled trial is warranted to confirm the effectiveness of this technique.
In conclusion, this prospective study evaluated the safety and effectiveness of opening window fistulotomy as a novel precutting method in patients with a large papillary roof. This new precutting technique displayed high safety with no complications of PEP or other major adverse events and a high success rate of CBD cannulation, indicating good feasibility as a means for primary biliary access. However, larger randomized controlled trials are required to validate our results in clinical settings.