INTRODUCTION
Endoscopic ultrasonography (EUS) has become an essential technique for the diagnosis of biliary and pancreatic diseases and is widely adopted worldwide. Recently, the use of EUS has expanded beyond just biliary and pancreatic diseases to allow detailed observation of the gastrointestinal tract and its adjacent organs. Procedures such as EUS-guided fine-needle aspiration (EUS-FNA) are being conducted, and genetic diagnoses based on this method are being performed. EUS has evolved from being merely diagnostic to therapeutic EUS. Although the oblique-viewing convex EUS (OV-EUS) is commonly used for therapeutic purposes, using the forward-viewing convex EUS (FV-EUS) can improve safety and overcome further challenges. In this review, we discuss the results of therapeutic EUS using the FV-EUS.
PROS AND CONS IN FV-EUS
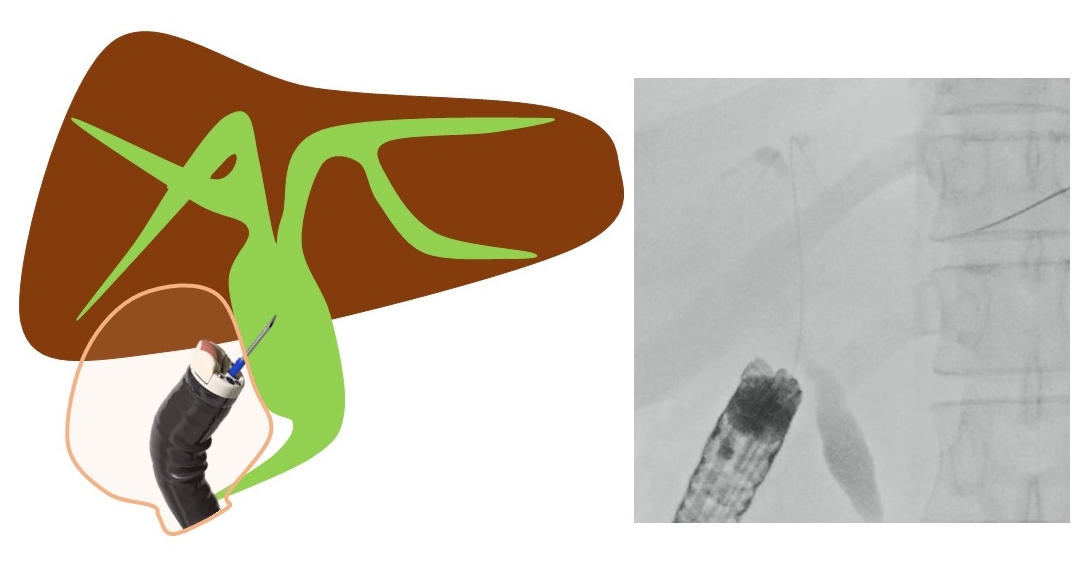
FV-EUS is an endoscopy technique that combines standard forward-viewing endoscopy with ultrasound imaging, allowing the physician to view the digestive tract and obtain high-quality ultrasound images of organs and lesions within or adjacent to the digestive tract. The forward-view allows for easy navigation through the gastrointestinal tract, which is especially beneficial for patients with surgically altered anatomy and accessing certain anatomical sites. FV-EUS also allows for vertical puncture in the gastrointestinal tract, leading to improved puncture performance.1 FV-EUS is highly useful for approaching areas that are difficult to reach with OV-EUS and when wanting to puncture the gastrointestinal tract vertically as shown in Figure 1 and Table 1. Cons of FV-EUS include its EUS imaging range being limited to 90┬░ and the absence of an elevator, which makes adjusting the puncture angle challenging.
EUS-GUIDED CHOLEDOCHODUODENOSTOMY
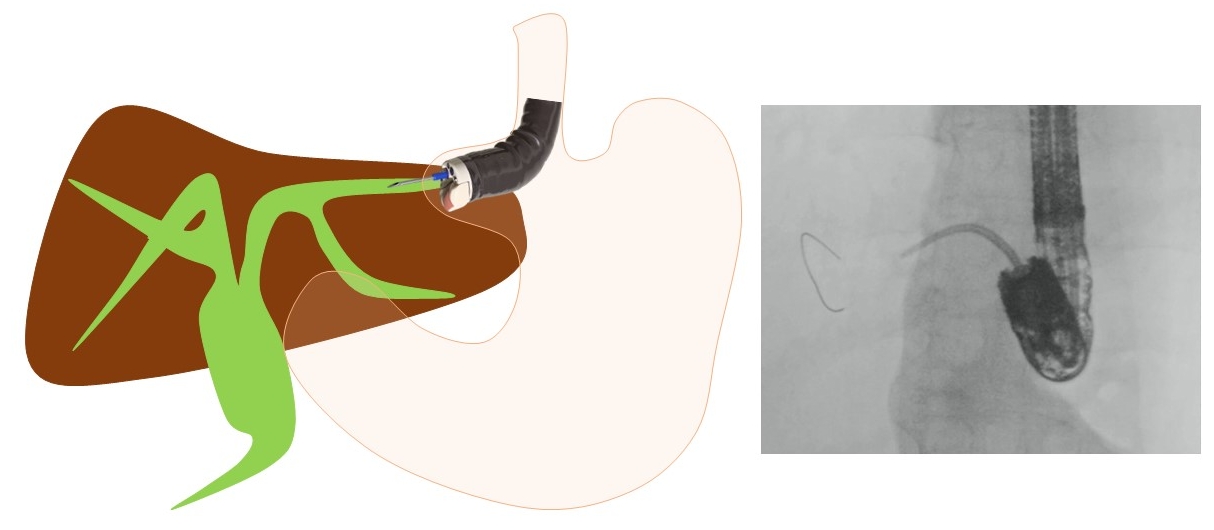
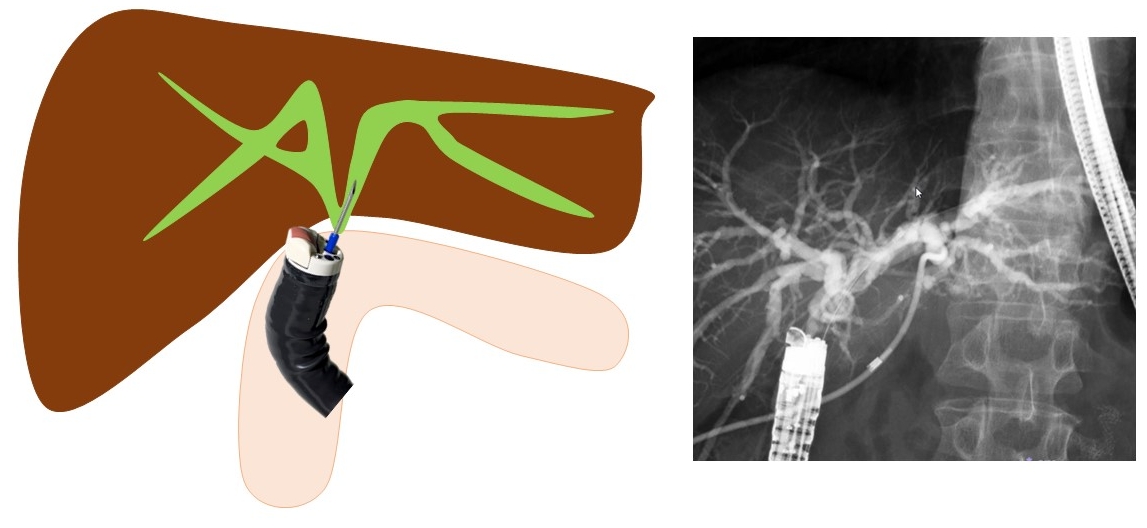
Hara et al. have reported a prospective study using FV-EUS for primary EUS-guided choledochoduodenostomy (EUS-CDS).2 This study describes the first prospective trial on primary EUS-guided biliary drainage and is the first study to examine the utility of FV-EUS in EUS-CDS. The technical and functional success rates were 94.4% (17/18) and 94.1% (16/17), respectively. Early adverse events (focal peritonitis) were encountered in 2 patients (11.8%). No patients developed late adverse events. These results are highly promising. Matsumoto et al.3 have reported that by using FV-EUS during EUS-CDS, double puncture of the digestive tract can be prevented. In OV-EUS, the axis of the scope and the puncture needle is different, resulting in the needle being inserted obliquely into the digestive tract, leading to a double puncture of the mucosa or difficulty in transmitting force.4 However, by using FV-EUS, these challenges can be overcome (Figs. 1, 2). When placing a stent, endoscopic imaging is easily available, allowing for the stent to be safely positioned in the appropriate position.1-3,5-7 For similar reasons, FV-EUS may also be useful for EUS-gallbladder drainage (EUS-GBD). It is believed that, by using FV-EUS, it is possible to avoid transgastric puncture and double puncture of the digestive tract mucosa in EUS-CDS and EUS-GBD. There are no reports summarizing the clinical outcomes of EUS-GBD.
EUS-GUIDED HEPATICOGASTROSTOMY
When performing EUS-guided hepaticogastrostomy (EUS-HGS), Hara and Okuno et al.8,9 first reported that, by using FV-EUS, a 22-G needle, and an 018 wire (Fig. 3), B2 puncture is available and the procedure becomes easier. When carrying out EUS-HGS, it is common to perform a B3 puncture to avoid transesophageal puncture. However, choosing B2 may be more convenient for tasks such as inserting the guidewire and some devices. If B2 can be punctured safely, it makes the procedure easier. According to a report by Okuno et al.,9 B2-EUS-HGS using FV-EUS has a success rate of 88.5% (54/61), with a complication rate of only 6.5% (4/61). There were no instances of transesophageal puncture. Moreover, Elshair et al.10 have reported the potential utility of techniques using FV-EUS when placing HGS in both B2 and B3.
EUS-GUIDED HEPATICOJEJUNOSTOMY
Kida et al.11 have first reported that in cases of EUS-guided hepaticojejunostomy (EUS-HJS), the bile duct is punctured using FV-EUS from the jejunum of the anastomosis, and a stent is placed (Fig. 4). Because the puncture is performed via the anastomosis, the risk of bile leakage is low, and drainage can be performed relatively safely. Although EUS-HGS can also treat anastomosis stenosis, it is difficult to drain the right side in cases where the left and right are separated. However, using this method, it is possible to drain both left and right hepatic ducts via the anastomosis. If a stent can be placed through the anastomosis, there is a possibility that the stent can ultimately be removed and made stent-free, and thus it is considered a first-line treatment method, especially in benign stenosis cases. Ishiwatari et al.12 reported that, in recurrent cases after pancreaticoduodenectomy, they performed EUS-HJS using FV-EUS from the afferent limb to drain the right bile duct of the liver. The limitation of this technique is the difficulty in inserting the FV-EUS up to the bile duct-jejunum anastomosis. These reports on EUS-HJS using FV-EUS are limited to case reports,11-20 and there are no published studies summarizing the clinical results. It is hoped that more extensive studies and reports will be conducted in the future.
EUS-GUIDED PANCREATICOJEJUNOSTOMY
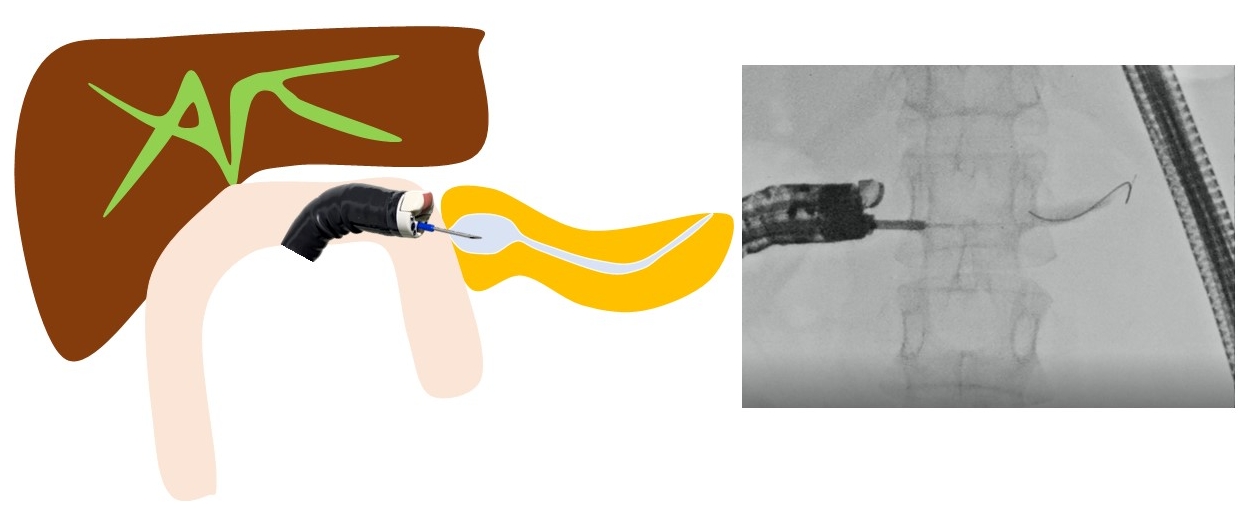
Endoscopic treatment for pancreatic duct-jejunum anastomosis stenosis is more challenging and prone to failure than that for bile duct-jejunum anastomosis stenosis. The gold standard is to dilate the anastomosis using a balloon endoscope and place a stent. However, if the usual method is challenging, treatment under EUS is effective. When using OV-EUS, it is common to approach from the stomach.21 However, there is no adhesion between the pancreas and stomach, which raises issues such as stent migration and misplacement, pancreatic fluid leakage, and pancreatitis. To address these problems, Nakaji et al.22 have reported on EUS-guided pancreaticojejunostomy (EUS-PJS). EUS-PJS is a technique that involves placing a pancreatic duct stent via the anastomosis and through the small intestine.11,21-27 Because there is a lower risk of postoperative stent misplacement into the abdominal cavity or pancreatic fluid leakage, it can be safely performed (Fig. 5). When inserting the stent via the stomach, in some cases, the guidewire cannot penetrate the anastomosis, necessitating permanent stent replacement. However, if approached through the anastomosis, there is a possibility to make it stent-free. These reports on EUS-PJS using FV-EUS have been limited to case reports,22-27 and there are no published studies summarizing the clinical results. More comprehensive studies and reports are anticipated in the future.
EUS-GUIDED PANCREATIC CYST DRAINAGE
EUS-guided pancreatic cyst drainage using EUS-FV was first reported by Voermans et al.28 It is believed that there are advantages to utilizing the endoscopic capabilities characteristic of FV. It is possible to treat digestive tract stenosis, visualize the stent after placement, and other options.1,7,29-32 However, because there is no difference in the technical and clinical success rate of this technique, the benefits of using FV-EUS seem to be limited.
OTHER TREATMENTS
Other reported treatments include drainage for intra-abdominal abscess (Fig. 6), liver abscess, splenic abscess, and endovascular treatments for gastric varices.33-38 FV-EUS may be used if it is possible to insert the endoscope deeply into the digestive tract, if puncturing perpendicularly to the digestive tract is feasible, and if endoscopic images are useful for the procedures.
CONCLUSIONS
FV-EUS presents a significant advancement in the field of gastrointestinal endoscopy, combining the advantages of both standard endoscopy and ultrasound imaging. Although it may not entirely replace traditional OV-EUS owing to certain limitations, its specific applications and advantages make it a valuable tool in both diagnostic and therapeutic endoscopy.