CME for
KSGE members
Gong and Bang: Whitish gastric mucosa on upper gastrointestinal endoscopy
Quiz
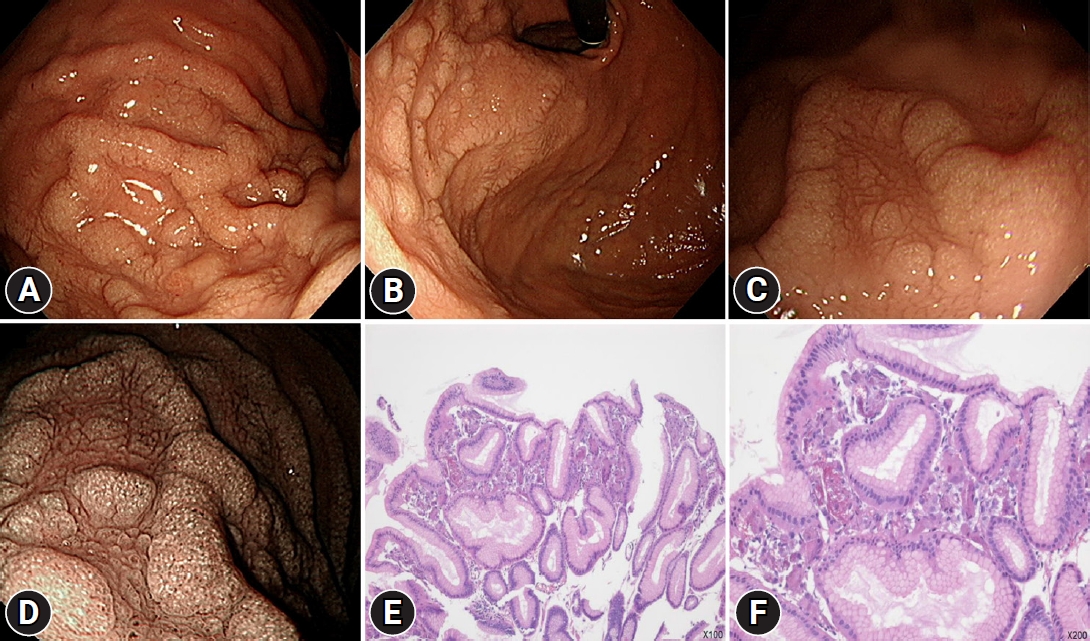
A 60-year-old man with hypertension and chronic glomerulonephritis visited the gastroenterology department for upper gastrointestinal endoscopy. He has been undergoing continuous ambulatory peritoneal dialysis for the past 8 years. He denied having any symptoms, and the vital signs were normal. On laboratory tests, the serum levels of hemoglobin, calcium, phosphorus, blood urea nitrogen, and creatinine were 9.8 g/dL, 9.5 mg/dL, 4.9 mg/dL, 71.3 mg/dL, and 11.8 mg/dL, respectively. His current medications are olmesartan, felodipine, lanthanum carbonate, calcitriol, cinacalcet hydrochloride, atorvastatin, darbepoetin alfa, and multi-vitamins. Endoscopy revealed diffuse whitish granular mucosa on the greater curvature side, posterior wall of the high body, and cardia ( Fig. 1Aт D). The patient had no Helicobacter pylori infection. What is the most likely diagnosis?
Answer 
Lanthanum carbonate is a phosphate-binding agent used to manage and treat hyperphosphatemia caused by end-stage renal disease. Since 2005, lanthanum carbonate has been available in the United States. 1 Generally, this insoluble complex is considered safe and poorly absorbed by the gastrointestinal tract. 2 Lanthanum deposition in the gastrointestinal tract was first described in 2015. 3 However, its clinical significance is uncertain. An association between gastric lanthanum carbonate deposition and mucosal atrophy has been postulated. The appearance and location of gastric lanthanum carbonate deposition on endoscopy may vary according to the extent of the gastric mucosal atrophy. In patients without gastric mucosal atrophy, lanthanum deposition appears as diffuse white lesions in the posterior wall and lesser curvature of the gastric body. Contrastingly, lanthanum-related lesions are likely to appear as annular or granular whitish lesions in patients with gastric mucosal atrophy. Moreover, these white lesions are more frequently observed in the lower part of the stomach, wherein intestinal metaplasia begins. 4 In this case, mucosal lesions are found on the greater curvature, posterior wall of the high body, and cardia without background mucosal atrophy. Differential diagnoses include gastric mucosal calcinosis, foveolar epithelial hyperplasia, and gastric intestinal metaplasia. 4-8 Endoscopic findings alone are often insufficient for definitive diagnosis, necessitating histopathological examination and a detailed history, including prescription information. According to a retrospective study, the total dose of lanthanum was significantly correlated with lanthanum deposition in the gastric mucosa. 9 This patient has been undergoing dialysis for >8 years, and the total dose of lanthanum is expected to be high to show gastric lanthanum deposition. Histopathologically, accumulation of macrophages containing fine, granular, and eosinophilic materials (phagocytosed deposits) can be observed in the lamina propria. In this case, histiocytes aggregating in superficial lamina propria, suggesting lanthanum deposition, was also found ( Fig. 1E, F) and has been considered as the bodyтs normal reaction to foreign bodies (deposition). 9 Immunohistochemical staining, such as anti-CD68 and CD206 staining, can be positive, implicating that M2 macrophages may be important in the clearance of lanthanum from the gastroduodenal mucosa. 10
Gastric lanthanum deposition is considered to not cause clinical symptoms and may be safe to use in patients with chronic kidney disease undergoing hemodialysis. 9 In this case, we describe diffuse whitish granular mucosa that should be differentiated from intestinal metaplasia in the stomach.
Fig.Т 1.
Endoscopic and histologic findings. (AтC) Diffuse whitish granular mucosa on the greater curvature side, posterior wall side of high body, and cardia on white-light imaging. (D) Diffuse whitish granular mucosa on the greater curvature side, posterior wall side of high body, and cardia on narrow-band imaging. (E, F) Histiocytes aggregating in superficial lamina propria (hematoxylin & eosin stain: E, У100; F, У200). 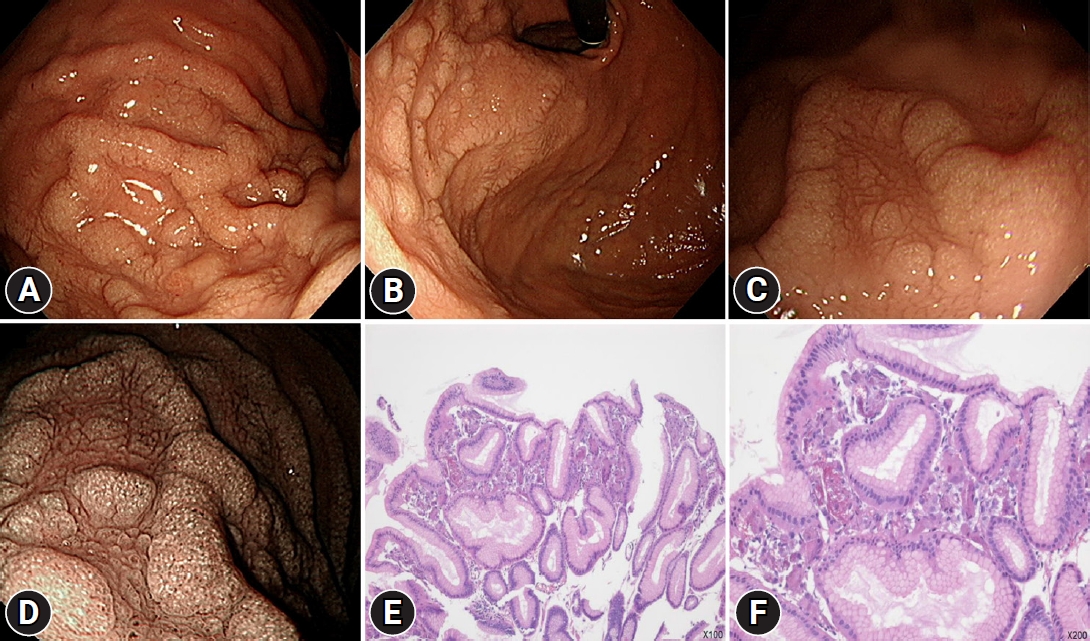
|
|